Back

Poster Session D - Tuesday Morning
Category: Liver
D0517 - Impact of Time and Location of Diagnostic Paracentesis on Outcomes of Spontaneous Bacterial Peritonitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- SM
Sriya Muralidharan, MD
Duke University
Durham, NC
Presenting Author(s)
Sriya Muralidharan, MD, Sukrit Jain, MD, Alice Parish, MSPH, Donna Niedzwiecki, PhD, Yuval Patel, MD
Duke University, Durham, NC
Introduction: Prior evidence demonstrates higher inpatient mortality in hospitalized patients with cirrhosis and ascites who undergo diagnostic paracentesis 12 hours after first physician encounter. However, the initial location of patient presentation and its impact on time to paracentesis has not been thoroughly studied. This analysis compared outcomes in patients with Spontaneous Bacterial Peritonitis (SBP) by location, either in the Emergency Department (ED) or the Internal Medicine (IM) floor, and timeliness of paracentesis.
Methods: We performed a retrospective cohort analysis of all patients aged 18 and older admitted to Duke University Health System (Duke Hospital, Duke Regional Hospital, Duke Raleigh Hospital) from 2018 to 2020 for decompensated cirrhosis who were diagnosed with SBP after paracentesis. We excluded patients who were incarcerated, had ascites from a non-hepatobiliary source, or were presumptively diagnosed with SBP without paracentesis. Chi square tests assessed the association between time to and location of paracentesis with patient outcomes including appropriate administration of albumin and mortality. Timeliness was categorically organized by < 12 hours or ≥12 hours to paracentesis. Location was defined as paracentesis done in the ED or by the IM team.
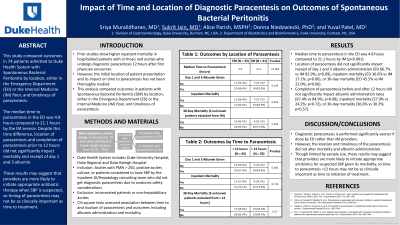
Results: 76 patients were included, of whom 33 had paracenteses performed by the ED, 41 by the IM service, and 2 by the surgical service. The median time to paracentesis in the ED was 4.8 hours compared to 21.1 hours by IM (p< 0.001). The location of paracentesis did not significantly impact receipt of day 1 and 3 albumin administration (ED 66.7% vs IM 82.9%; p=0.09), inpatient mortality (ED 36.6% vs IM 17.1%; p=0.06), or 30-day mortality (ED 45.5% vs IM 22.0%; p=0.06). Completion of paracentesis before and after 12 hours did not significantly impact albumin administration rates (67.4% vs 84.9%; p=0.08), inpatient mortality (27.9% vs 24.2%; p=0.72), or 30-day mortality (36.6% vs 30.3%; p=0.57).
Discussion: Diagnostic paracentesis is performed significantly sooner if done by ED rather than IM providers. However, the location and timeliness of the paracentesis did not alter mortality and albumin administration. Though limited by sample size, these results may suggest that providers are more likely to initiate appropriate antibiotics for suspected SBP given its morbidity, so time to paracentesis < 12 hours may not be as clinically important as time to initiation of treatment.
Disclosures:
Sriya Muralidharan, MD, Sukrit Jain, MD, Alice Parish, MSPH, Donna Niedzwiecki, PhD, Yuval Patel, MD. D0517 - Impact of Time and Location of Diagnostic Paracentesis on Outcomes of Spontaneous Bacterial Peritonitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Duke University, Durham, NC
Introduction: Prior evidence demonstrates higher inpatient mortality in hospitalized patients with cirrhosis and ascites who undergo diagnostic paracentesis 12 hours after first physician encounter. However, the initial location of patient presentation and its impact on time to paracentesis has not been thoroughly studied. This analysis compared outcomes in patients with Spontaneous Bacterial Peritonitis (SBP) by location, either in the Emergency Department (ED) or the Internal Medicine (IM) floor, and timeliness of paracentesis.
Methods: We performed a retrospective cohort analysis of all patients aged 18 and older admitted to Duke University Health System (Duke Hospital, Duke Regional Hospital, Duke Raleigh Hospital) from 2018 to 2020 for decompensated cirrhosis who were diagnosed with SBP after paracentesis. We excluded patients who were incarcerated, had ascites from a non-hepatobiliary source, or were presumptively diagnosed with SBP without paracentesis. Chi square tests assessed the association between time to and location of paracentesis with patient outcomes including appropriate administration of albumin and mortality. Timeliness was categorically organized by < 12 hours or ≥12 hours to paracentesis. Location was defined as paracentesis done in the ED or by the IM team.
Results: 76 patients were included, of whom 33 had paracenteses performed by the ED, 41 by the IM service, and 2 by the surgical service. The median time to paracentesis in the ED was 4.8 hours compared to 21.1 hours by IM (p< 0.001). The location of paracentesis did not significantly impact receipt of day 1 and 3 albumin administration (ED 66.7% vs IM 82.9%; p=0.09), inpatient mortality (ED 36.6% vs IM 17.1%; p=0.06), or 30-day mortality (ED 45.5% vs IM 22.0%; p=0.06). Completion of paracentesis before and after 12 hours did not significantly impact albumin administration rates (67.4% vs 84.9%; p=0.08), inpatient mortality (27.9% vs 24.2%; p=0.72), or 30-day mortality (36.6% vs 30.3%; p=0.57).
Discussion: Diagnostic paracentesis is performed significantly sooner if done by ED rather than IM providers. However, the location and timeliness of the paracentesis did not alter mortality and albumin administration. Though limited by sample size, these results may suggest that providers are more likely to initiate appropriate antibiotics for suspected SBP given its morbidity, so time to paracentesis < 12 hours may not be as clinically important as time to initiation of treatment.
Disclosures:
Sriya Muralidharan indicated no relevant financial relationships.
Sukrit Jain indicated no relevant financial relationships.
Alice Parish indicated no relevant financial relationships.
Donna Niedzwiecki indicated no relevant financial relationships.
Yuval Patel indicated no relevant financial relationships.
Sriya Muralidharan, MD, Sukrit Jain, MD, Alice Parish, MSPH, Donna Niedzwiecki, PhD, Yuval Patel, MD. D0517 - Impact of Time and Location of Diagnostic Paracentesis on Outcomes of Spontaneous Bacterial Peritonitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
