Back

Poster Session D - Tuesday Morning
Category: Liver
D0518 - Health Inequalities in NAFLD Distribution and Outcomes: A Nationwide Analysis Over a Decade
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Sophia H. Dar, MD
Hackensack University Medical Center
South Amboy, NJ
Presenting Author(s)
Sophia H. Dar, MD1, Maryam Haider, MD2, Nooraldin Merza, MD3, Yousaf Zafar, 4, Rosario H. Ligresti, MD5
1Hackensack University Medical Center, South Amboy, NJ; 2Wayne State University/Detroit Medical Center Sinai Grace Hospital, Detroit, MI; 3Wayne State University Medical Center, Detroit, MI; 4University of Mississippi Medical Center, Madison, MS; 5Hackensack University Medical Center, Hackensack, NJ
Introduction: Non-Alcoholic Liver Disease (NAFLD) is becoming progressively more prevalent as obesity and DM rise. The massive burden of disease owing to NAFLD has necessitated an effort to understand better the epidemiological, history, and progression of the disease. However, we know little about the distribution of health inequalities in NAFLD. We aim to review and analyze these health disparities and trends over the last decade.
Methods: We conduct a retrospective review of the national inpatient sample from 2008 through 2018. We extracted patient and institutional characteristics directly from the database. International classification of disease (ICD) codes identified variables, including NAFLD. We used the Chi-square test to analyze continuous variables and multivariate logistic regression to analyze independent predictors of mortality, total hospital charges, and length of stay.
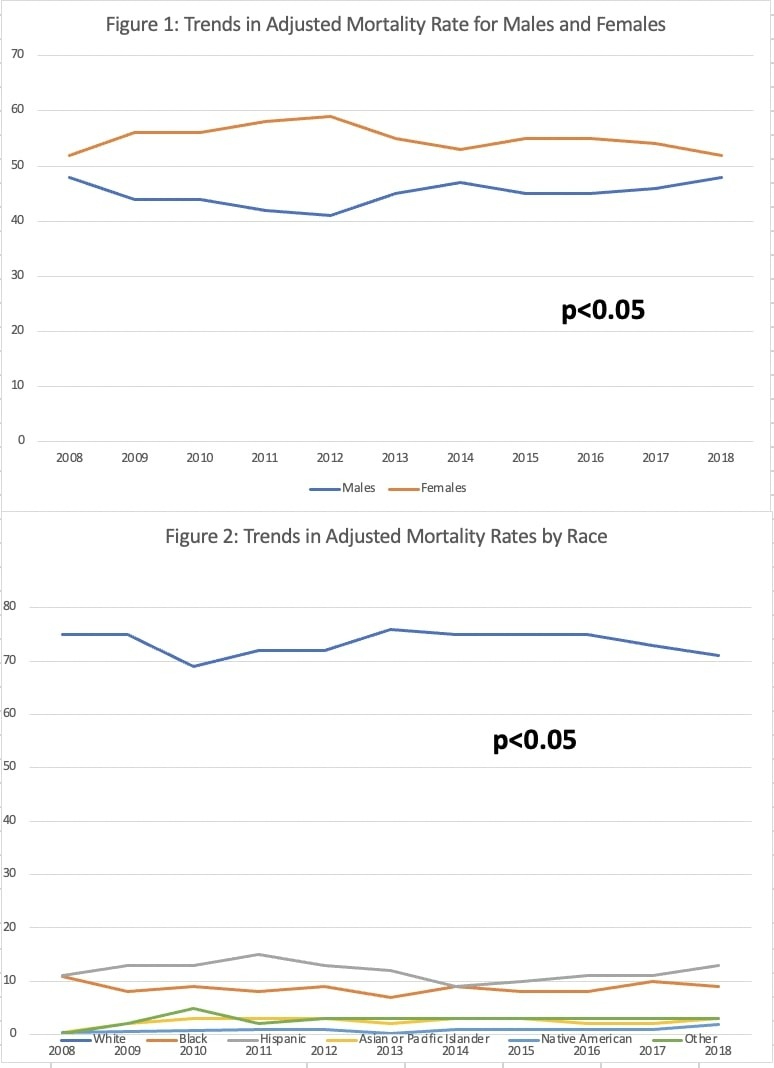
Results: A total of 2,473,982 NAFLD patients are included in this analysis, out of which 234,533 survived, and 2,239,449 had died over the ten years. The mean age of mortality is higher than the mean survival age (63 vs. 55 p< 0.05). Females had a higher percentage of NAFLD that both survived (56% vs. 44% p< 0.05) and died (54% vs. 46% p< 0.05) compared to males. Females also had decreased odds of mortality compared to males [0.94 (0.89-0.96) p< 0.05]. Whites were the most common race and were also noted to have an increased mortality rate (70% vs. 73%). Interestingly, Hispanics had a higher rate of survival (15% vs. 12% p< 0.05) and had lower odds of mortality compared to Whites [0.86 (0.8-0.93) p< 0.05]. NAFLD patients with a Charlson Comorbidity Index of 3 or more had a significantly higher mortality rate than those who survived (70% vs. 33% p< 0.05). Teaching hospitals had lower mortality rates than non-teaching hospitals (32% vs. 68%). Trends over ten years showed that both Whites and females had a decreasing mortality rate over the decade as seen in Figures 1 and 2 respectively.
Discussion: Multiple health disparities exist between patients with NAFLD, and these health inequalities affect mortality outcomes. Whites and females have higher rates of prevalence and mortality, while females and Hispanics were both found to have lower odds of mortality. Concomitant comorbidities play a significant role in mortality in this patient population, as does teaching versus non-teaching hospital admission. These findings can help us better educate our scientists, physicians, and leaders to improve care for this population.
Disclosures:
Sophia H. Dar, MD1, Maryam Haider, MD2, Nooraldin Merza, MD3, Yousaf Zafar, 4, Rosario H. Ligresti, MD5. D0518 - Health Inequalities in NAFLD Distribution and Outcomes: A Nationwide Analysis Over a Decade, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Hackensack University Medical Center, South Amboy, NJ; 2Wayne State University/Detroit Medical Center Sinai Grace Hospital, Detroit, MI; 3Wayne State University Medical Center, Detroit, MI; 4University of Mississippi Medical Center, Madison, MS; 5Hackensack University Medical Center, Hackensack, NJ
Introduction: Non-Alcoholic Liver Disease (NAFLD) is becoming progressively more prevalent as obesity and DM rise. The massive burden of disease owing to NAFLD has necessitated an effort to understand better the epidemiological, history, and progression of the disease. However, we know little about the distribution of health inequalities in NAFLD. We aim to review and analyze these health disparities and trends over the last decade.
Methods: We conduct a retrospective review of the national inpatient sample from 2008 through 2018. We extracted patient and institutional characteristics directly from the database. International classification of disease (ICD) codes identified variables, including NAFLD. We used the Chi-square test to analyze continuous variables and multivariate logistic regression to analyze independent predictors of mortality, total hospital charges, and length of stay.
Results: A total of 2,473,982 NAFLD patients are included in this analysis, out of which 234,533 survived, and 2,239,449 had died over the ten years. The mean age of mortality is higher than the mean survival age (63 vs. 55 p< 0.05). Females had a higher percentage of NAFLD that both survived (56% vs. 44% p< 0.05) and died (54% vs. 46% p< 0.05) compared to males. Females also had decreased odds of mortality compared to males [0.94 (0.89-0.96) p< 0.05]. Whites were the most common race and were also noted to have an increased mortality rate (70% vs. 73%). Interestingly, Hispanics had a higher rate of survival (15% vs. 12% p< 0.05) and had lower odds of mortality compared to Whites [0.86 (0.8-0.93) p< 0.05]. NAFLD patients with a Charlson Comorbidity Index of 3 or more had a significantly higher mortality rate than those who survived (70% vs. 33% p< 0.05). Teaching hospitals had lower mortality rates than non-teaching hospitals (32% vs. 68%). Trends over ten years showed that both Whites and females had a decreasing mortality rate over the decade as seen in Figures 1 and 2 respectively.
Discussion: Multiple health disparities exist between patients with NAFLD, and these health inequalities affect mortality outcomes. Whites and females have higher rates of prevalence and mortality, while females and Hispanics were both found to have lower odds of mortality. Concomitant comorbidities play a significant role in mortality in this patient population, as does teaching versus non-teaching hospital admission. These findings can help us better educate our scientists, physicians, and leaders to improve care for this population.
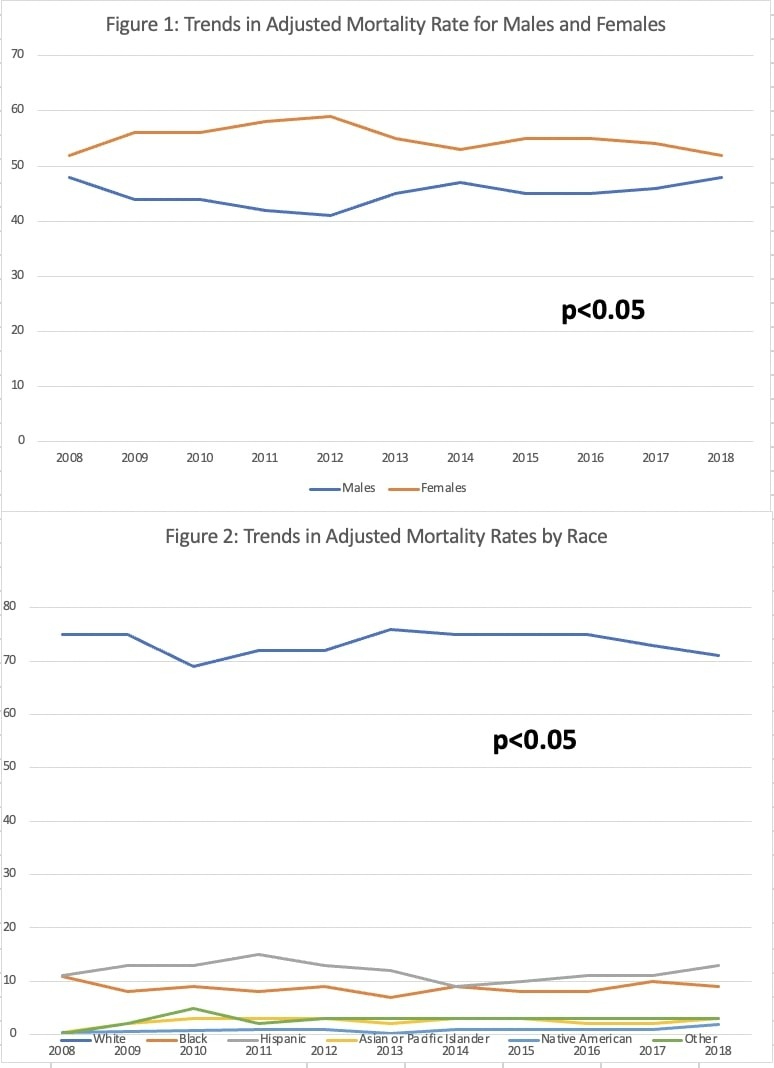
Figure: Figure 1: Trends in adjusted mortality for males and females
Figure 2: Trends in adjusted mortality rates by race
Figure 2: Trends in adjusted mortality rates by race
Disclosures:
Sophia Dar indicated no relevant financial relationships.
Maryam Haider indicated no relevant financial relationships.
Nooraldin Merza indicated no relevant financial relationships.
Yousaf Zafar indicated no relevant financial relationships.
Rosario Ligresti indicated no relevant financial relationships.
Rosario Ligresti — NO DISCLOSURE DATA.
Sophia H. Dar, MD1, Maryam Haider, MD2, Nooraldin Merza, MD3, Yousaf Zafar, 4, Rosario H. Ligresti, MD5. D0518 - Health Inequalities in NAFLD Distribution and Outcomes: A Nationwide Analysis Over a Decade, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
