Back

Poster Session B - Monday Morning
Category: IBD
B0424 - Capecitabine-Induced Ileitis vs Late-Onset Crohn’s Disease: A Case Report
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kavitha Vijayasekar, MD
Icahn School of Medicine at Mount Sinai (Emlhurst) Hospital
Omaha, NE
Presenting Author(s)
Bryce Schutte, DO1, Kavitha Vijayasekar, MD2, Erin Jenkins, MD1
1CHI Creighton University Medical Center, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Ileitis is most commonly thought to be related to Crohn’s disease. Other causes do exist, including infection, vasculopathy, ischemia, neoplasm, medication induced, and eosinophilia. Proper diagnosis relies upon clinical course, systemic manifestations, appearance on imaging and endoscopy, and histological analysis. Making the correct diagnosis is integral to management of the underlying disease. Here we present a case of long segment ileitis caused by capecitabine vs late-onset Crohn’s disease.
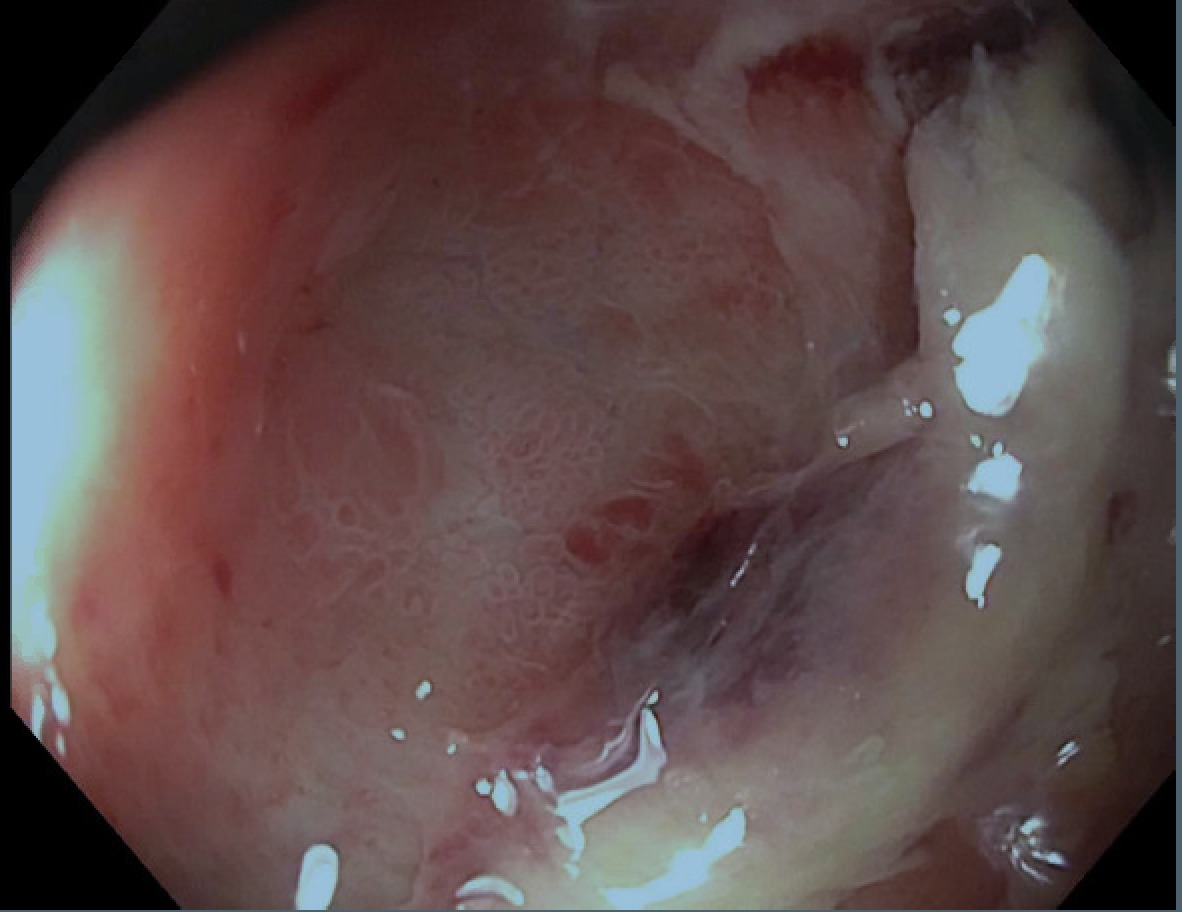
Case Description/Methods: A 72 y.o. male with a history of cholangiocarcinoma (CCA) who had left hepatic lobe trisegmentectomy and Roux-en-Y hepaticojejunostomy with lymphadenectomy followed by chemotherapy with capecitabine 3 months later. He was admitted for nausea and vomiting 2 months after this was initiated. CT abdomen revealed distal ileitis with upstream distention. A colonoscopy was performed, showing severe inflammation with ulceration in the terminal ileum. Biopsies showed chronic active inflammation and cryptitis with crypt abscesses, concerning for Crohn’s disease. MRI enterography showed long segment ileitis. He began a prednisone taper, and capecitabine was stopped. He clinically improved and was discharged home. At follow-up in GI clinic, his symptoms had significantly improved. Because of the temporal association between the initiation of capecitabine and the patient’s symptoms, the decision was made to monitor the patient clinically and only consider starting biologic agents if he had persistent symptoms and endoscopic findings consistent with Crohn’s disease.
Discussion: This case illustrates the potential overlap between chemotherapy induced ileitis and Crohn’s disease. Our patient had a history of CCA, but hepatic resection did not show evidence of primary sclerosing cholangitis (PSC). Previous ERCP did show dilation of the common bile duct and intrahepatic bile ducts, but this may have been related to his malignancy. Because of the correlation between CCA, PSC, and inflammatory bowel disease, this makes Crohn’s disease a likely possibility. However, there have been multiple cases of capecitabine induced ileitis in the literature. Patients with capecitabine induced ileitis were found to improve with discontinuation of the medication and occasionally steroids whereas Crohn’s Disease would require additional therapy with biologic agents. The proper diagnosis is integral to treatment, so further evaluation is indicated.
Disclosures:
Bryce Schutte, DO1, Kavitha Vijayasekar, MD2, Erin Jenkins, MD1. B0424 - Capecitabine-Induced Ileitis vs Late-Onset Crohn’s Disease: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1CHI Creighton University Medical Center, Omaha, NE; 2Creighton University, Omaha, NE
Introduction: Ileitis is most commonly thought to be related to Crohn’s disease. Other causes do exist, including infection, vasculopathy, ischemia, neoplasm, medication induced, and eosinophilia. Proper diagnosis relies upon clinical course, systemic manifestations, appearance on imaging and endoscopy, and histological analysis. Making the correct diagnosis is integral to management of the underlying disease. Here we present a case of long segment ileitis caused by capecitabine vs late-onset Crohn’s disease.
Case Description/Methods: A 72 y.o. male with a history of cholangiocarcinoma (CCA) who had left hepatic lobe trisegmentectomy and Roux-en-Y hepaticojejunostomy with lymphadenectomy followed by chemotherapy with capecitabine 3 months later. He was admitted for nausea and vomiting 2 months after this was initiated. CT abdomen revealed distal ileitis with upstream distention. A colonoscopy was performed, showing severe inflammation with ulceration in the terminal ileum. Biopsies showed chronic active inflammation and cryptitis with crypt abscesses, concerning for Crohn’s disease. MRI enterography showed long segment ileitis. He began a prednisone taper, and capecitabine was stopped. He clinically improved and was discharged home. At follow-up in GI clinic, his symptoms had significantly improved. Because of the temporal association between the initiation of capecitabine and the patient’s symptoms, the decision was made to monitor the patient clinically and only consider starting biologic agents if he had persistent symptoms and endoscopic findings consistent with Crohn’s disease.
Discussion: This case illustrates the potential overlap between chemotherapy induced ileitis and Crohn’s disease. Our patient had a history of CCA, but hepatic resection did not show evidence of primary sclerosing cholangitis (PSC). Previous ERCP did show dilation of the common bile duct and intrahepatic bile ducts, but this may have been related to his malignancy. Because of the correlation between CCA, PSC, and inflammatory bowel disease, this makes Crohn’s disease a likely possibility. However, there have been multiple cases of capecitabine induced ileitis in the literature. Patients with capecitabine induced ileitis were found to improve with discontinuation of the medication and occasionally steroids whereas Crohn’s Disease would require additional therapy with biologic agents. The proper diagnosis is integral to treatment, so further evaluation is indicated.
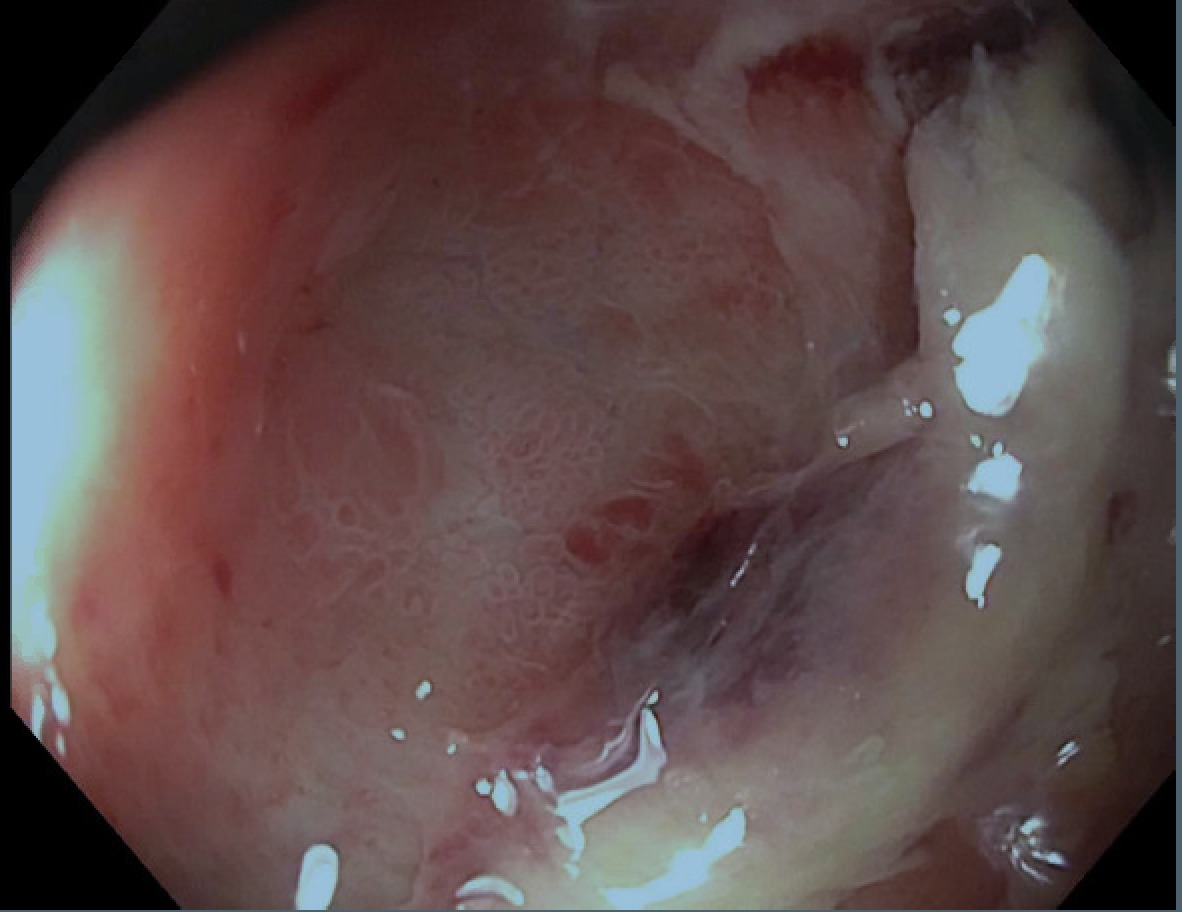
Figure: Terminal Ileum Ulcer
Disclosures:
Bryce Schutte indicated no relevant financial relationships.
Kavitha Vijayasekar indicated no relevant financial relationships.
Erin Jenkins indicated no relevant financial relationships.
Bryce Schutte, DO1, Kavitha Vijayasekar, MD2, Erin Jenkins, MD1. B0424 - Capecitabine-Induced Ileitis vs Late-Onset Crohn’s Disease: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
