Back

Poster Session D - Tuesday Morning
Category: IBD
D0425 - Heart Aches With Mesalamine: A Rare Case of Aminosalicylate-Induced Myopericarditis in a Basic Military Trainee
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- CC
Christopher M. Cowan, MD
Brooke Army Medical Center
Fort Sam Houston, TX
Presenting Author(s)
Christopher M. Cowan, MD1, Geoffrey A. Bader, MD2
1Brooke Army Medical Center, Fort Sam Houston, TX; 2SAUSHEC, San Antonio, TX
Introduction: Ulcerative Colitis (UC) is a chronic autoimmune condition predominately manifesting as colonic inflammation with serious morbidity. Early intervention with medical therapies can alter the disease course, improving symptoms and reducing the need for hospitalization and surgery. While patients and providers are increasingly focused on the use and side effects of biologic therapies, older medications such as mesalamine (5-ASA) are still commonly prescribed and can cause idiosyncratic reactions. We present a case of 5-ASA induced myopericarditis to highlight this rare, life threatening complication.
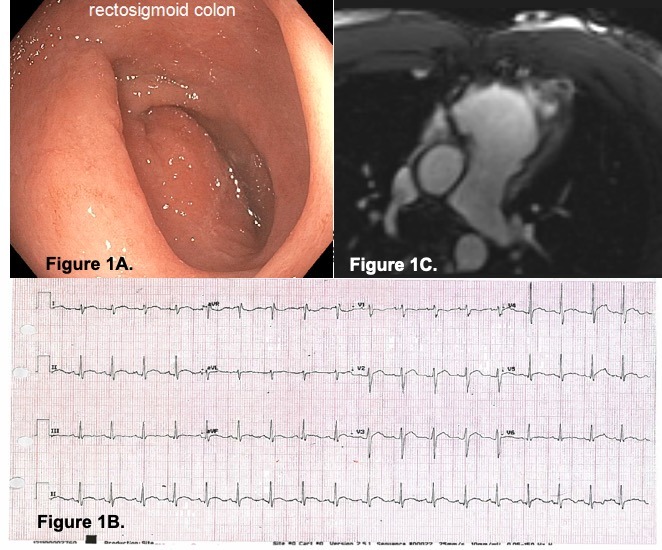
Case Description/Methods: A 28 year old male basic military trainee was referred for evaluation of iron deficiency anemia. Patient reported chronic 2-4 bowel movements daily and hematochezia with wiping. Physical exam was unremarkable. Labs revealed hemoglobin of 11.6g/dL, iron saturation 15% and ferritin 16ng/mL. The patient underwent colonoscopy, which demonstrated features consistent with Mayo 2 UC extending from the anus to 30cm (Figure 1a), with biopsies confirming chronic active proctitis and colitis. Patient was started on oral 5-ASA for mildly active left sided UC with good clinical response. Three weeks after starting treatment, patient presented to the Emergency Department with pleuritic chest pain, worse with exertion. Electrocardiogram (EKG) showed diffusely elevated T waves (Figure 2). Labs revealed a troponin of 0.03ng/mL and proBrain natriuretic peptide of 1888pg/mL. Patient was admitted to the hospital and ruled out for alternative infectious and autoimmune etiologies. Cardiac MRI demonstrated diffuse, patchy ventricular enhancement and a reduced left ventricular systolic function (Figure 3). Patient was diagnosed with 5-ASA induced myopericarditis and discharged on colchicine and prednisone with good clinical response.
Discussion: Myopericarditis is a rare, potentially lethal complication of 5-ASA therapy. The pathophysiology of 5-ASA related cardiac manifestations are poorly understood, with reactions typically seen within the first 1-4 weeks of treatment. Diagnosis of 5-ASA pericarditis is clinical without distinguishing features from other causes of pericarditis. Most patients improve dramatically with discontinuation and lifelong avoidance of mesalamine, with the role for steroids and anti-inflammatory therapy somewhat controversial. Our case serves to remind clinicians of this serious side effect and the importance of thorough risk-benefits counseling for any UC treatment.
Disclosures:
Christopher M. Cowan, MD1, Geoffrey A. Bader, MD2. D0425 - Heart Aches With Mesalamine: A Rare Case of Aminosalicylate-Induced Myopericarditis in a Basic Military Trainee, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brooke Army Medical Center, Fort Sam Houston, TX; 2SAUSHEC, San Antonio, TX
Introduction: Ulcerative Colitis (UC) is a chronic autoimmune condition predominately manifesting as colonic inflammation with serious morbidity. Early intervention with medical therapies can alter the disease course, improving symptoms and reducing the need for hospitalization and surgery. While patients and providers are increasingly focused on the use and side effects of biologic therapies, older medications such as mesalamine (5-ASA) are still commonly prescribed and can cause idiosyncratic reactions. We present a case of 5-ASA induced myopericarditis to highlight this rare, life threatening complication.
Case Description/Methods: A 28 year old male basic military trainee was referred for evaluation of iron deficiency anemia. Patient reported chronic 2-4 bowel movements daily and hematochezia with wiping. Physical exam was unremarkable. Labs revealed hemoglobin of 11.6g/dL, iron saturation 15% and ferritin 16ng/mL. The patient underwent colonoscopy, which demonstrated features consistent with Mayo 2 UC extending from the anus to 30cm (Figure 1a), with biopsies confirming chronic active proctitis and colitis. Patient was started on oral 5-ASA for mildly active left sided UC with good clinical response. Three weeks after starting treatment, patient presented to the Emergency Department with pleuritic chest pain, worse with exertion. Electrocardiogram (EKG) showed diffusely elevated T waves (Figure 2). Labs revealed a troponin of 0.03ng/mL and proBrain natriuretic peptide of 1888pg/mL. Patient was admitted to the hospital and ruled out for alternative infectious and autoimmune etiologies. Cardiac MRI demonstrated diffuse, patchy ventricular enhancement and a reduced left ventricular systolic function (Figure 3). Patient was diagnosed with 5-ASA induced myopericarditis and discharged on colchicine and prednisone with good clinical response.
Discussion: Myopericarditis is a rare, potentially lethal complication of 5-ASA therapy. The pathophysiology of 5-ASA related cardiac manifestations are poorly understood, with reactions typically seen within the first 1-4 weeks of treatment. Diagnosis of 5-ASA pericarditis is clinical without distinguishing features from other causes of pericarditis. Most patients improve dramatically with discontinuation and lifelong avoidance of mesalamine, with the role for steroids and anti-inflammatory therapy somewhat controversial. Our case serves to remind clinicians of this serious side effect and the importance of thorough risk-benefits counseling for any UC treatment.
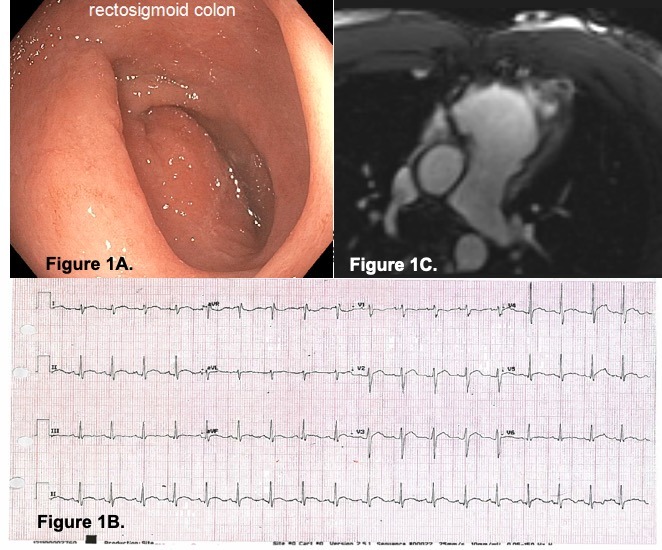
Figure: Figure 1. Fig 1A: Colonoscopy images showing erythema, vascular drop out, small erosions, and contact friability consistent with Mayo 2 UC. Fig 2B: EKG demonstrating diffuse T wave elevations consistent with Pericarditis. Fig 2C: Cardiac MRI demonstrating diffuse, patchy left ventricular gadolinium enhancement.
Disclosures:
Christopher Cowan indicated no relevant financial relationships.
Geoffrey Bader indicated no relevant financial relationships.
Christopher M. Cowan, MD1, Geoffrey A. Bader, MD2. D0425 - Heart Aches With Mesalamine: A Rare Case of Aminosalicylate-Induced Myopericarditis in a Basic Military Trainee, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
