Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0719 - A Rare Case of Phlegmonous Gastritis in a Previously Healthy Male
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Omar Masarweh, MD
University of Central Florida- HCA Healthcare GME
Kissimmee, FL
Presenting Author(s)
Omar Masarweh, MD1, Raj Shah, MD2, Feras Al-Moussally, MD3, Andy Huang, 4, Basher Atiquzzaman, MD5
1University of Central Florida- HCA Healthcare GME, Kissimmee, FL; 2University of Central Florida HCA Healthcare GME, Kissimmee, FL; 3University of Central Florida - HCA Healthcare GME, Kissimmee, FL; 4University of Central Florida College of Medicine, Kissimmee, FL; 5Digestive and Liver Center of Florida, Kissimmee, FL
Introduction: Phlegmonous gastritis (PG) is a rare and often fatal disease characterized by severe bacterial invasion of the gastric wall.1 Due to its rarity and subtle clinical manifestations early diagnosis is difficult, causing delays in identification and treatment leading to increased mortality.2 We present a case of a previously healthy male who developed PG and responded well to antibiotics.
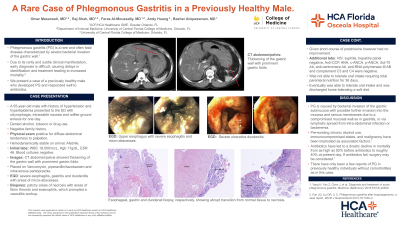
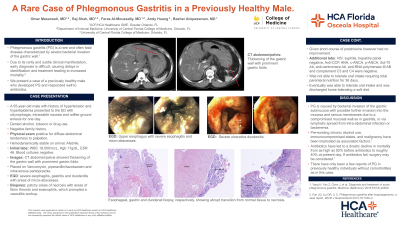
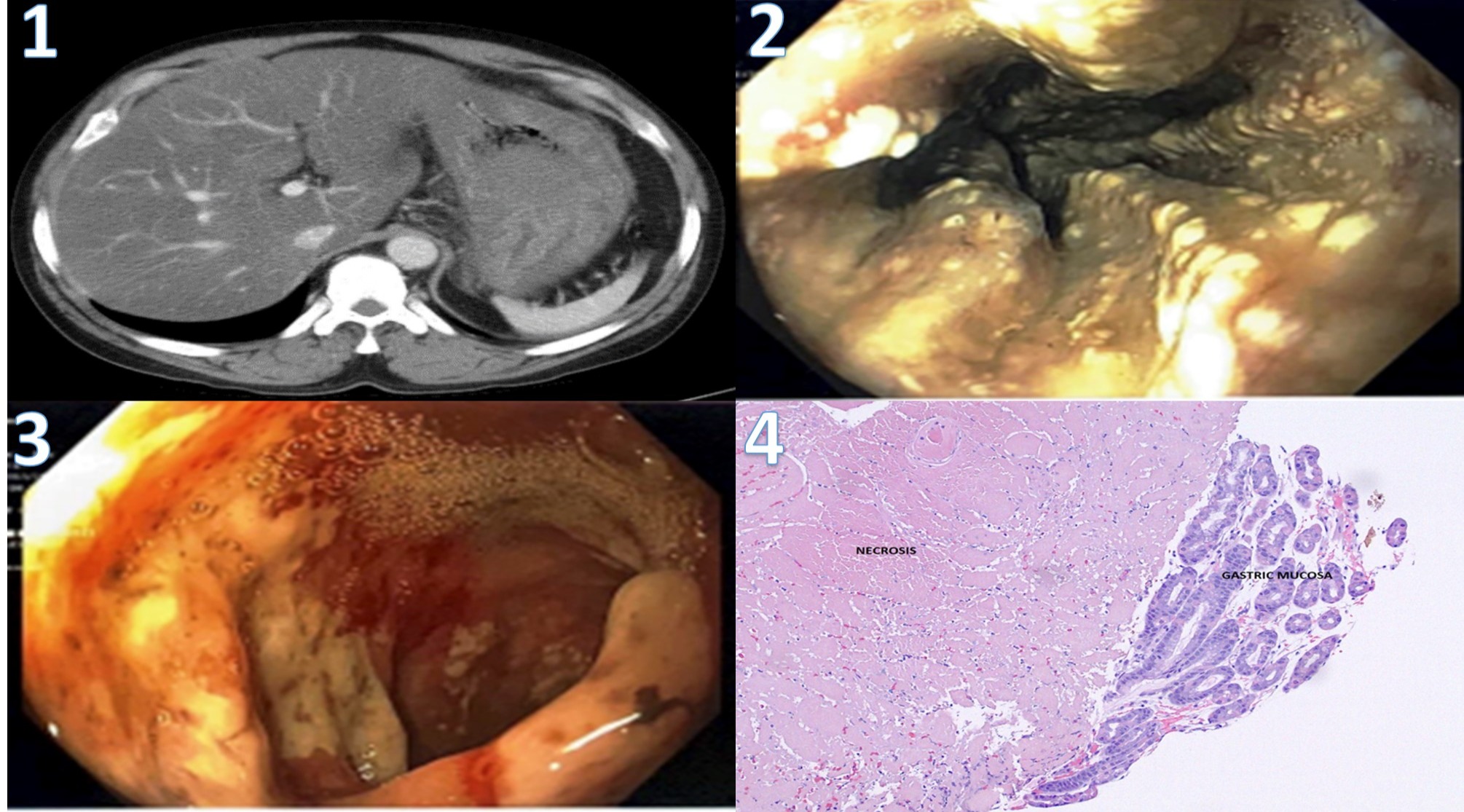
Case Description/Methods: A 55-year-old male with history of hypertension and hyperlipidemia presented to an emergency room with odynophagia, intractable nausea, and coffee ground emesis for one day. On arrival, he was hemodynamically stable, afebrile, and labs showed a white count of 19,500/mcL, hemoglobin 17g/dL, ESR 46mm/hr, and negative for HIV, syphilis, and hepatitis. Blood cultures were negative. CT abdomen showed thickening of the gastric wall with prominent gastric folds (figure 1). He was started on vancomycin, piperacillin/tazobactam, and pantoprazole. EGD demonstrated severe esophagitis, gastritis, and ulcerative duodenitis with prominent gastric folds and excessive purulent debris with areas of micro-abscesses (figure 2-3). Biopsies showed necrosis in the esophagus, stomach and duodenum with areas of fibrin thrombi and eosinophils (figure 4-6). Immunochemical and special stains were negative for H. pylori, CD 68, CMV, congo red, and PAS. Vasculitis was considered due to the areas of patchy necrosis, but anti-CCP, ANA, c-ANCA, p-ANCA, Scl-70 Ab, anti-centromere Ab, anti-RNA polymerase III Ab, and complement C3 and C4 were negative, with rheumatoid factor elevated at 15 InU/mL (normal 0-12). During his hospital stay he received broad-spectrum antibiotics, prednisone, and required total parenteral nutrition for 36 days until he was able to tolerate oral intake, then he was discharged home tolerating a soft diet.
Discussion: PG is caused by bacterial invasion of the gastric submucosa with possible further invasion into the mucosa and serous membranes due to a compromised mucosal wall as in gastritis, or via lymphatic spread from intra-abdominal infections or bacteremia. Pre-existing chronic alcohol use, immunocompromised states, and malignancy have been implicated as associated factors.1 There have been only a few reports of PG in previously healthy individuals without comorbidities as in this case. Antibiotics have led to drastic decline in mortality from as high as 92% before the advent of antibiotics to roughly 42% at present day.1 If medical management is ineffective, surgery may be performed.
Disclosures:
Omar Masarweh, MD1, Raj Shah, MD2, Feras Al-Moussally, MD3, Andy Huang, 4, Basher Atiquzzaman, MD5. A0719 - A Rare Case of Phlegmonous Gastritis in a Previously Healthy Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Central Florida- HCA Healthcare GME, Kissimmee, FL; 2University of Central Florida HCA Healthcare GME, Kissimmee, FL; 3University of Central Florida - HCA Healthcare GME, Kissimmee, FL; 4University of Central Florida College of Medicine, Kissimmee, FL; 5Digestive and Liver Center of Florida, Kissimmee, FL
Introduction: Phlegmonous gastritis (PG) is a rare and often fatal disease characterized by severe bacterial invasion of the gastric wall.1 Due to its rarity and subtle clinical manifestations early diagnosis is difficult, causing delays in identification and treatment leading to increased mortality.2 We present a case of a previously healthy male who developed PG and responded well to antibiotics.
Case Description/Methods: A 55-year-old male with history of hypertension and hyperlipidemia presented to an emergency room with odynophagia, intractable nausea, and coffee ground emesis for one day. On arrival, he was hemodynamically stable, afebrile, and labs showed a white count of 19,500/mcL, hemoglobin 17g/dL, ESR 46mm/hr, and negative for HIV, syphilis, and hepatitis. Blood cultures were negative. CT abdomen showed thickening of the gastric wall with prominent gastric folds (figure 1). He was started on vancomycin, piperacillin/tazobactam, and pantoprazole. EGD demonstrated severe esophagitis, gastritis, and ulcerative duodenitis with prominent gastric folds and excessive purulent debris with areas of micro-abscesses (figure 2-3). Biopsies showed necrosis in the esophagus, stomach and duodenum with areas of fibrin thrombi and eosinophils (figure 4-6). Immunochemical and special stains were negative for H. pylori, CD 68, CMV, congo red, and PAS. Vasculitis was considered due to the areas of patchy necrosis, but anti-CCP, ANA, c-ANCA, p-ANCA, Scl-70 Ab, anti-centromere Ab, anti-RNA polymerase III Ab, and complement C3 and C4 were negative, with rheumatoid factor elevated at 15 InU/mL (normal 0-12). During his hospital stay he received broad-spectrum antibiotics, prednisone, and required total parenteral nutrition for 36 days until he was able to tolerate oral intake, then he was discharged home tolerating a soft diet.
Discussion: PG is caused by bacterial invasion of the gastric submucosa with possible further invasion into the mucosa and serous membranes due to a compromised mucosal wall as in gastritis, or via lymphatic spread from intra-abdominal infections or bacteremia. Pre-existing chronic alcohol use, immunocompromised states, and malignancy have been implicated as associated factors.1 There have been only a few reports of PG in previously healthy individuals without comorbidities as in this case. Antibiotics have led to drastic decline in mortality from as high as 92% before the advent of antibiotics to roughly 42% at present day.1 If medical management is ineffective, surgery may be performed.
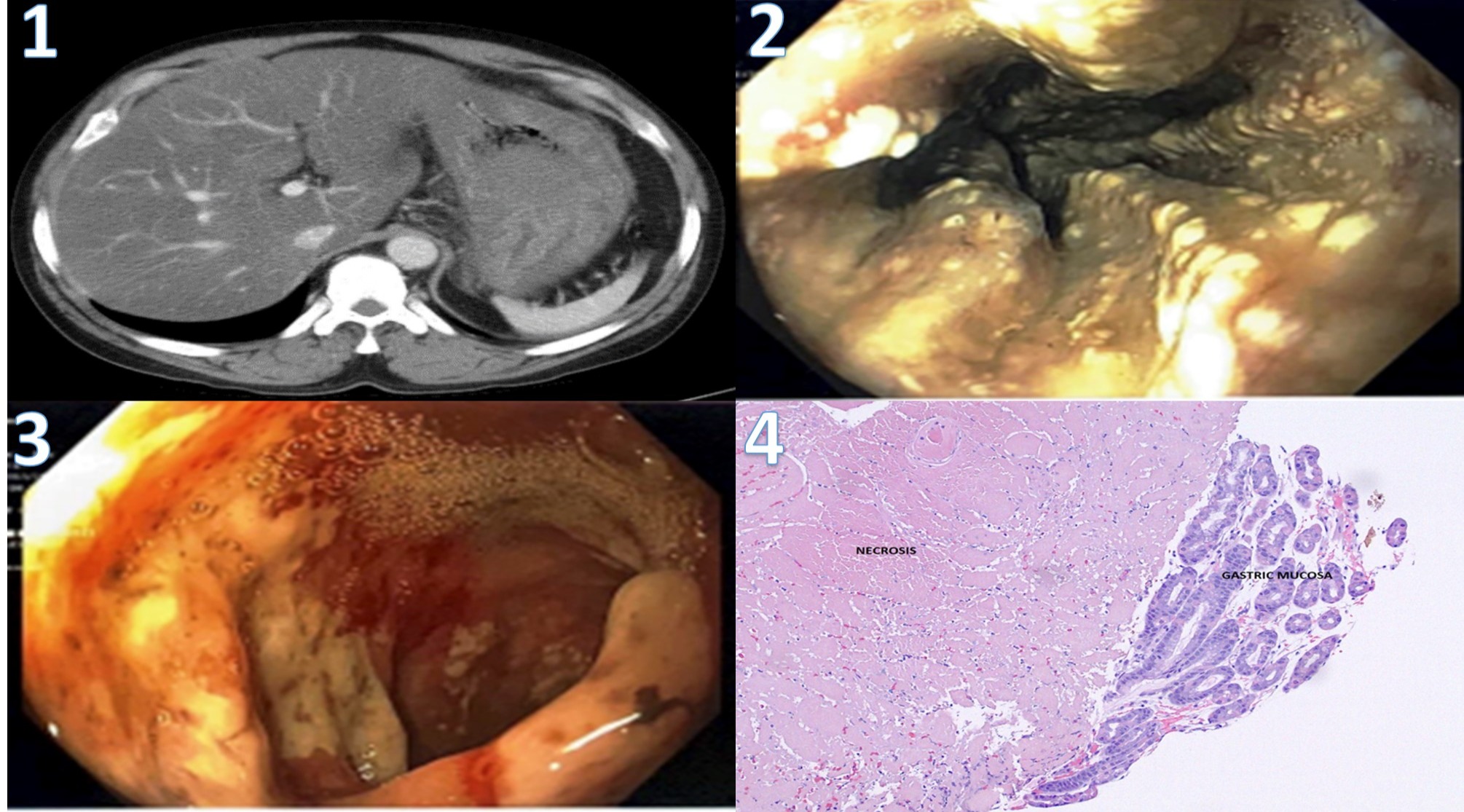
Figure: Figures
Disclosures:
Omar Masarweh indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Feras Al-Moussally indicated no relevant financial relationships.
Andy Huang indicated no relevant financial relationships.
Basher Atiquzzaman indicated no relevant financial relationships.
Omar Masarweh, MD1, Raj Shah, MD2, Feras Al-Moussally, MD3, Andy Huang, 4, Basher Atiquzzaman, MD5. A0719 - A Rare Case of Phlegmonous Gastritis in a Previously Healthy Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
