Back

Poster Session B - Monday Morning
Category: GI Bleeding
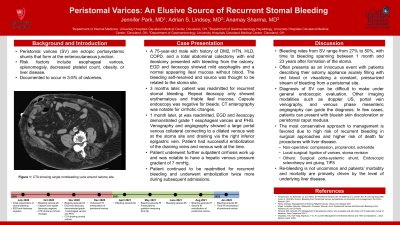
B0334 - Peristomal Varices: An Elusive Source of Recurrent Stomal Bleeding
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
Jennifer Park, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Jennifer Park, MD1, Adrian Lindsey, MD2, Anamay Sharma, MD3
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals, Cleveland, OH; 3Cleveland VA Medical Center, Cleveland, OH
Introduction: Peristomal varices are thought to be caused from abnormal communications between the high-pressure portal system and relatively low-pressure systemic circulation. It can be a source of recurrent bleeding and can be difficult to diagnose with endoscopic evaluation.
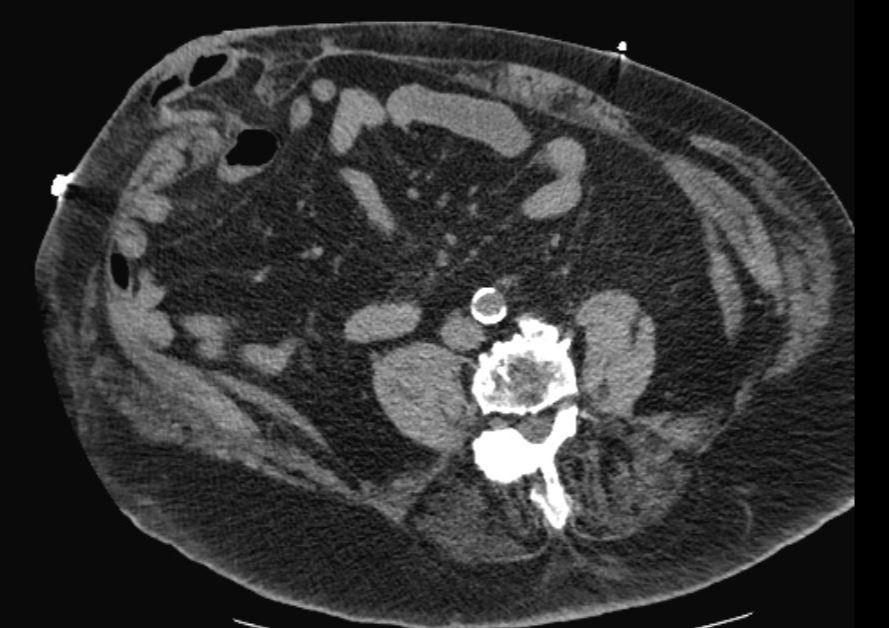
Case Description/Methods: A 75-year-old male with history of a total abdominal colectomy with end ileostomy due to severe sigmoid diverticular stricture presented with bleeding from the ostomy. EGD and ileoscopy showed mild esophagitis and a normal appearing ileal mucosa without blood. The bleeding self-resolved and source was thought to be related to the stoma site. 3 months later, patient was readmitted for recurrent stomal bleeding. Repeat ileoscopy only showed erythematous and friable ileal mucosa. Capsule endoscopy was negative for bleeds. Once again, the bleeding self-resolved. He was readmitted one month later and had been undergoing outpatient cirrhosis work up. EGD and ileoscopy demonstrated grade 1 esophageal varices and PHG. Venography and angiography showed a large portal venous collateral connecting to a dilated venous web at the stoma site and draining via the right inferior epigastric vein. Patient underwent successful embolization of the draining veins and venous web at the time and twice more during subsequent admissions.
Discussion: Peristomal varices (SV) have been documented to occur in 3-5% of ostomies with bleeding rates ranging from 27% to 50%, and time to bleeding spanning between 1 month and 23 years after formation of the stoma. Risk factors include esophageal varices, splenomegaly, decreased platelet count, obesity, or liver disease. The diagnosis can be difficult to make as unlike other ectopic varices within the GI tract, SVs are not usually visible to the naked eye and their shallow location are often not visible under general endoscopic evaluation. Other imaging modalities such as doppler US, portal vein venography, and venous phase mesenteric angiography can guide the diagnosis. In few cases, patients can present with blueish skin discoloration or peristomal caput medusa. The most conservative approach to management is favored due to high risk of recurrent bleeding in surgical approaches and higher risk of death for procedures with liver disease. Re-bleeding is not uncommon and patients’ morbidity and mortality are primarily driven by the level of underlying liver disease. In conclusion, SV can be a differential in cases of recurrent stomal bleeds without an identifiable source on endoscopic evaluation.
Disclosures:
Jennifer Park, MD1, Adrian Lindsey, MD2, Anamay Sharma, MD3. B0334 - Peristomal Varices: An Elusive Source of Recurrent Stomal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals, Cleveland, OH; 3Cleveland VA Medical Center, Cleveland, OH
Introduction: Peristomal varices are thought to be caused from abnormal communications between the high-pressure portal system and relatively low-pressure systemic circulation. It can be a source of recurrent bleeding and can be difficult to diagnose with endoscopic evaluation.
Case Description/Methods: A 75-year-old male with history of a total abdominal colectomy with end ileostomy due to severe sigmoid diverticular stricture presented with bleeding from the ostomy. EGD and ileoscopy showed mild esophagitis and a normal appearing ileal mucosa without blood. The bleeding self-resolved and source was thought to be related to the stoma site. 3 months later, patient was readmitted for recurrent stomal bleeding. Repeat ileoscopy only showed erythematous and friable ileal mucosa. Capsule endoscopy was negative for bleeds. Once again, the bleeding self-resolved. He was readmitted one month later and had been undergoing outpatient cirrhosis work up. EGD and ileoscopy demonstrated grade 1 esophageal varices and PHG. Venography and angiography showed a large portal venous collateral connecting to a dilated venous web at the stoma site and draining via the right inferior epigastric vein. Patient underwent successful embolization of the draining veins and venous web at the time and twice more during subsequent admissions.
Discussion: Peristomal varices (SV) have been documented to occur in 3-5% of ostomies with bleeding rates ranging from 27% to 50%, and time to bleeding spanning between 1 month and 23 years after formation of the stoma. Risk factors include esophageal varices, splenomegaly, decreased platelet count, obesity, or liver disease. The diagnosis can be difficult to make as unlike other ectopic varices within the GI tract, SVs are not usually visible to the naked eye and their shallow location are often not visible under general endoscopic evaluation. Other imaging modalities such as doppler US, portal vein venography, and venous phase mesenteric angiography can guide the diagnosis. In few cases, patients can present with blueish skin discoloration or peristomal caput medusa. The most conservative approach to management is favored due to high risk of recurrent bleeding in surgical approaches and higher risk of death for procedures with liver disease. Re-bleeding is not uncommon and patients’ morbidity and mortality are primarily driven by the level of underlying liver disease. In conclusion, SV can be a differential in cases of recurrent stomal bleeds without an identifiable source on endoscopic evaluation.
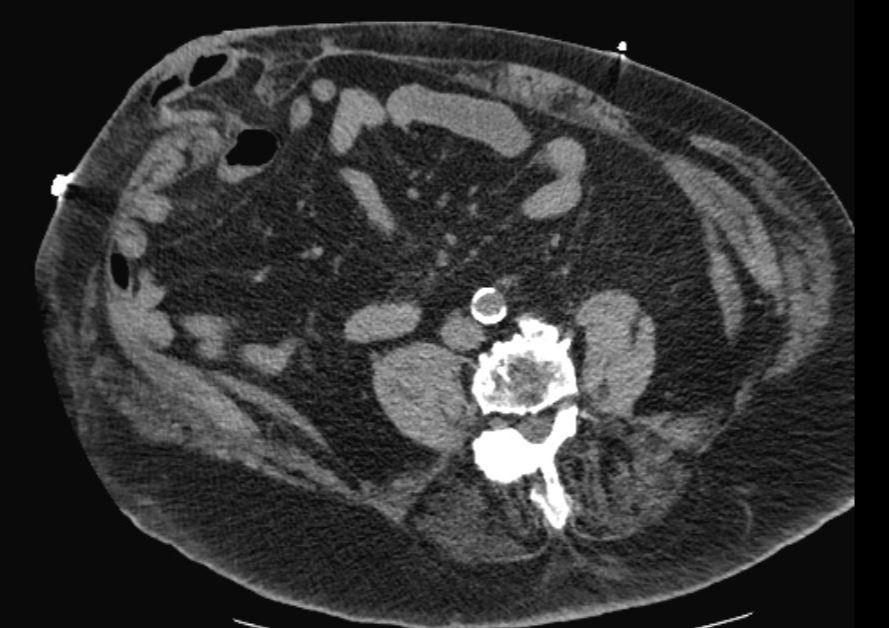
Figure: Peristomal varix demonstrated on CT scan
Disclosures:
Jennifer Park indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Anamay Sharma indicated no relevant financial relationships.
Jennifer Park, MD1, Adrian Lindsey, MD2, Anamay Sharma, MD3. B0334 - Peristomal Varices: An Elusive Source of Recurrent Stomal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

