Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0658 - Autoimmune Enteropathy: A Rare Cause of Small Intestinal Villous Atrophy in Adults
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Katelin M. Durham, MD
University of Iowa Hospitals and Clinics
Iowa City, IA
Presenting Author(s)
Katelin M. Durham, MD1, Steven Polyak, MD1, Joseph Laakman, MD1, Aditi Reddy, MD2, Xiaocen Zhang, MD3
1University of Iowa Hospitals and Clinics, Iowa City, IA; 2UIHC, Iowa City, IA; 3University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Autoimmune enteropathy (AIE) is a rare cause of small intestinal villous atrophy. This condition is more frequently diagnosed in children, with only a handful of case series describing its presentation in adults. We present a case of adult-onset AIE in which diagnosis was made based on its unique endoscopic and histologic findings.
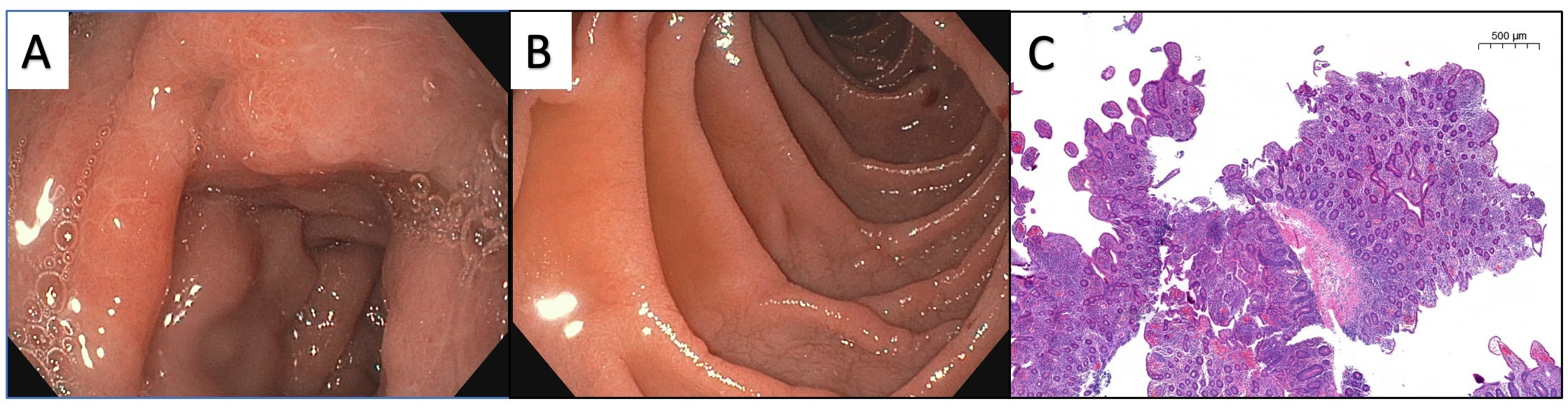
Case Description/Methods: A 54 year-old previously healthy woman was hospitalized with profuse watery diarrhea, abdominal pain, and weight loss of six months duration. Stool testing was negative for infection. Inflammatory markers were mildly elevated. Computer tomography imaging showed hyperenhancement of the small bowel consistent with enteritis, without evidence of stricture or abscess. She underwent esophagogastroduodenoscopy which revealed diffuse edema of the duodenal mucosa with villous blunting and cracked-earth appearance (Figure 1A, 1B). She had normal appearing mucosa of the distal small bowel and colon on video capsule endoscopy and colonoscopy, respectively. Pathology from duodenal biopsies showed chronic active duodenitis characterized by marked villous blunting, reduced goblet and Paneth cells, neutrophilic and lymphocytic infiltration of deep crypts, and basal layer apoptosis (Figure 1C). Similar findings were seen in random ileal biopsies, while random colon biopsies were normal. Anti-enterocyte antibodies and anti-transglutaminase antibodies were negative. Patient was treated for AIE with intravenous methylprednisolone and she required supplemental parental nutrition. Within days of initiating steroids, her diarrhea had improved and she was transitioned to oral prednisone. Several days later she was weaned off parenteral nutrition and stable for discharge with plans to introduce a thiopurine at follow-up.
Discussion: AIE should be suspected in a patient with chronic diarrhea, signs of severe malabsorption, and characteristic histologic features in absence of other causes of villous atrophy such as Celiac disease. Specific histologic features of AIE include absence of goblet cells and Paneth cells and presence of crypt apoptotic bodies in intestinal biopsies. Development of autoantibodies against enterocytes are associated with this condition, but not required for diagnosis. Steroids are the mainstay of therapy and have variable effect. We aim to raise awareness of AIE, as the rarity of this condition can make its diagnosis elusive.
Disclosures:
Katelin M. Durham, MD1, Steven Polyak, MD1, Joseph Laakman, MD1, Aditi Reddy, MD2, Xiaocen Zhang, MD3. D0658 - Autoimmune Enteropathy: A Rare Cause of Small Intestinal Villous Atrophy in Adults, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Iowa Hospitals and Clinics, Iowa City, IA; 2UIHC, Iowa City, IA; 3University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Autoimmune enteropathy (AIE) is a rare cause of small intestinal villous atrophy. This condition is more frequently diagnosed in children, with only a handful of case series describing its presentation in adults. We present a case of adult-onset AIE in which diagnosis was made based on its unique endoscopic and histologic findings.
Case Description/Methods: A 54 year-old previously healthy woman was hospitalized with profuse watery diarrhea, abdominal pain, and weight loss of six months duration. Stool testing was negative for infection. Inflammatory markers were mildly elevated. Computer tomography imaging showed hyperenhancement of the small bowel consistent with enteritis, without evidence of stricture or abscess. She underwent esophagogastroduodenoscopy which revealed diffuse edema of the duodenal mucosa with villous blunting and cracked-earth appearance (Figure 1A, 1B). She had normal appearing mucosa of the distal small bowel and colon on video capsule endoscopy and colonoscopy, respectively. Pathology from duodenal biopsies showed chronic active duodenitis characterized by marked villous blunting, reduced goblet and Paneth cells, neutrophilic and lymphocytic infiltration of deep crypts, and basal layer apoptosis (Figure 1C). Similar findings were seen in random ileal biopsies, while random colon biopsies were normal. Anti-enterocyte antibodies and anti-transglutaminase antibodies were negative. Patient was treated for AIE with intravenous methylprednisolone and she required supplemental parental nutrition. Within days of initiating steroids, her diarrhea had improved and she was transitioned to oral prednisone. Several days later she was weaned off parenteral nutrition and stable for discharge with plans to introduce a thiopurine at follow-up.
Discussion: AIE should be suspected in a patient with chronic diarrhea, signs of severe malabsorption, and characteristic histologic features in absence of other causes of villous atrophy such as Celiac disease. Specific histologic features of AIE include absence of goblet cells and Paneth cells and presence of crypt apoptotic bodies in intestinal biopsies. Development of autoantibodies against enterocytes are associated with this condition, but not required for diagnosis. Steroids are the mainstay of therapy and have variable effect. We aim to raise awareness of AIE, as the rarity of this condition can make its diagnosis elusive.
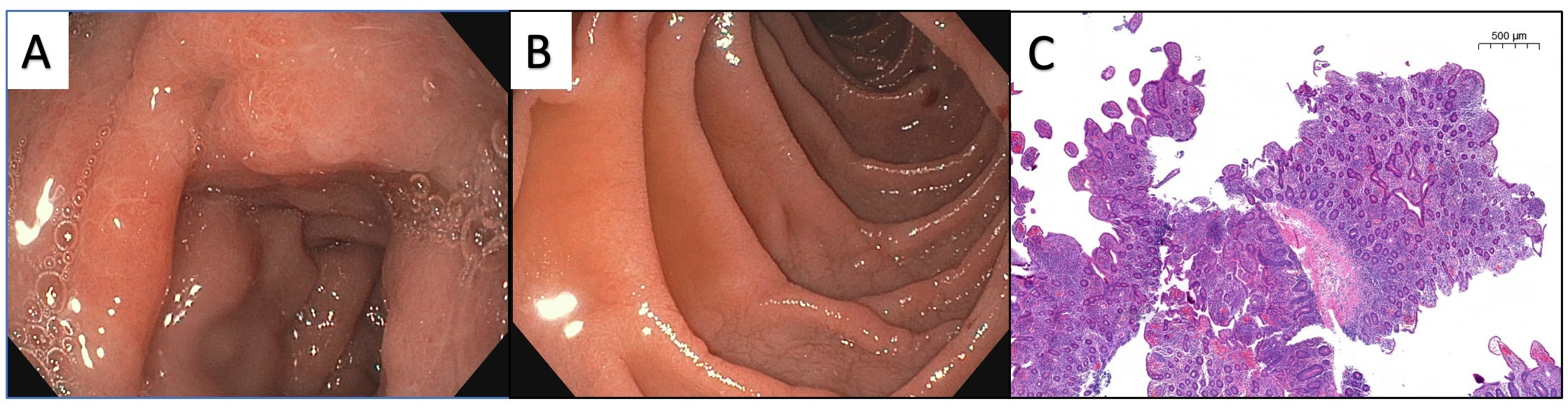
Figure: Figure 1A. EGD shows villous blunting and edema of duodenal mucosa.
Figure 1B. EGD shows cracked-earth appearance of duodenal mucosa.
Figure 1C. Duodenal biopsy reveals chronic active duodenitis characterized by marked villous blunting, reduced goblet and Paneth cells, neutrophilic and lymphocytic infiltration of deep crypts, and basal layer apoptosis.
Figure 1B. EGD shows cracked-earth appearance of duodenal mucosa.
Figure 1C. Duodenal biopsy reveals chronic active duodenitis characterized by marked villous blunting, reduced goblet and Paneth cells, neutrophilic and lymphocytic infiltration of deep crypts, and basal layer apoptosis.
Disclosures:
Katelin Durham indicated no relevant financial relationships.
Steven Polyak indicated no relevant financial relationships.
Joseph Laakman indicated no relevant financial relationships.
Aditi Reddy indicated no relevant financial relationships.
Xiaocen Zhang indicated no relevant financial relationships.
Katelin M. Durham, MD1, Steven Polyak, MD1, Joseph Laakman, MD1, Aditi Reddy, MD2, Xiaocen Zhang, MD3. D0658 - Autoimmune Enteropathy: A Rare Cause of Small Intestinal Villous Atrophy in Adults, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
