Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0660 - Iron Deficiency Anemia and Small Bowel Strictures: Thinking Beyond Crohn's Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Amanda Eisinger, DO
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Amanda Eisinger, DO, Vanessa Sostre-Santiago, MD, Gowthami Kanagalingam, MD, Abtin Jafroodifar, MD, Ramos, MD, Bishnu Sapkota, MD
SUNY Upstate Medical University, Syracuse, NY
Introduction: NSAIDs are well known to cause gastrointestinal (GI) mucosal damage. We present a case of a 72-year-old male who was found to have Diaphragm Disease (DD).
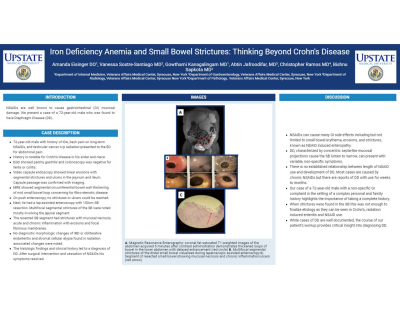
Case Description/Methods: 72-year-old male with history of IDA, back pain on long-term NSAIDs, and testicular cancer s/p radiation presented to the ED for abdominal pain. History is notable for Crohn’s disease in his sister and niece. EGD showed patchy gastritis and colonoscopy was negative for ileitis or colitis. Video capsule endoscopy showed linear erosions with segmental strictures and ulcers in the jejunum and ileum. Capsule passage was confirmed with imaging. MRE showed segmental circumferential bowel wall thickening of mid small bowel loop concerning for fibro-stenotic disease. On push enteroscopy, no strictures or ulcers could be reached. Next, he had a lap-assisted enteroscopy with 150cm SB resection. Multifocal segmental strictures of the SB were noted mostly involving the jejunal segment. The resected SB segment had strictures with mucosal necrosis, acute and chronic inflammation with erosions and focal fibrinous membranes. No diagnostic morphologic changes of IBD or obliterative endarteritis and stromal cellular atypia found in radiation associated changes were noted. The histologic findings and clinical history led to a diagnosis of DD. After surgical intervention and cessation of NSAIDs his symptoms resolved.
Discussion: NSAIDs can cause many GI side effects including but not limited to small bowel erythema, erosions, and strictures, known as NSAID induced enteropathy. DD, characterized by concentric septa-like mucosal projections cause the SB lumen to narrow, can present with variable, non-specific symptoms. There is no established relationship between length of NSAID use and development of DD. Most cases are caused by chronic NSAIDs but there are reports of DD with use for weeks to months. Our case of a 72-year-old male with a non-specific GI complaint in the setting of a complex personal and family history highlights the importance of taking a complete history. When strictures were found in the SB this was not enough to finalize etiology as they can be seen in Crohn’s, radiation induced enteritis and NSAID use. While cases of DD are well documented, the course of our patient’s workup provides critical insight into diagnosing DD.

Disclosures:
Amanda Eisinger, DO, Vanessa Sostre-Santiago, MD, Gowthami Kanagalingam, MD, Abtin Jafroodifar, MD, Ramos, MD, Bishnu Sapkota, MD. D0660 - Iron Deficiency Anemia and Small Bowel Strictures: Thinking Beyond Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
SUNY Upstate Medical University, Syracuse, NY
Introduction: NSAIDs are well known to cause gastrointestinal (GI) mucosal damage. We present a case of a 72-year-old male who was found to have Diaphragm Disease (DD).
Case Description/Methods: 72-year-old male with history of IDA, back pain on long-term NSAIDs, and testicular cancer s/p radiation presented to the ED for abdominal pain. History is notable for Crohn’s disease in his sister and niece. EGD showed patchy gastritis and colonoscopy was negative for ileitis or colitis. Video capsule endoscopy showed linear erosions with segmental strictures and ulcers in the jejunum and ileum. Capsule passage was confirmed with imaging. MRE showed segmental circumferential bowel wall thickening of mid small bowel loop concerning for fibro-stenotic disease. On push enteroscopy, no strictures or ulcers could be reached. Next, he had a lap-assisted enteroscopy with 150cm SB resection. Multifocal segmental strictures of the SB were noted mostly involving the jejunal segment. The resected SB segment had strictures with mucosal necrosis, acute and chronic inflammation with erosions and focal fibrinous membranes. No diagnostic morphologic changes of IBD or obliterative endarteritis and stromal cellular atypia found in radiation associated changes were noted. The histologic findings and clinical history led to a diagnosis of DD. After surgical intervention and cessation of NSAIDs his symptoms resolved.
Discussion: NSAIDs can cause many GI side effects including but not limited to small bowel erythema, erosions, and strictures, known as NSAID induced enteropathy. DD, characterized by concentric septa-like mucosal projections cause the SB lumen to narrow, can present with variable, non-specific symptoms. There is no established relationship between length of NSAID use and development of DD. Most cases are caused by chronic NSAIDs but there are reports of DD with use for weeks to months. Our case of a 72-year-old male with a non-specific GI complaint in the setting of a complex personal and family history highlights the importance of taking a complete history. When strictures were found in the SB this was not enough to finalize etiology as they can be seen in Crohn’s, radiation induced enteritis and NSAID use. While cases of DD are well documented, the course of our patient’s workup provides critical insight into diagnosing DD.

Figure: A. Magnetic Resonance Enterography: coronal fat saturated T1-weighted images of the abdomen acquired 5 minutes after contrast administration demonstrates thickened loops of bowel in the lower abdomen with delayed enhancement (red circle) B. Multifocal segmental strictures of the distal small bowel visualized during laparoscopic assisted enteroscopy C. Segment of resected small bowel showing mucosal necrosis and chronic inflammation/ulcers (red arrow)
Disclosures:
Amanda Eisinger indicated no relevant financial relationships.
Vanessa Sostre-Santiago indicated no relevant financial relationships.
Gowthami Kanagalingam indicated no relevant financial relationships.
Abtin Jafroodifar indicated no relevant financial relationships.
Ramos indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Amanda Eisinger, DO, Vanessa Sostre-Santiago, MD, Gowthami Kanagalingam, MD, Abtin Jafroodifar, MD, Ramos, MD, Bishnu Sapkota, MD. D0660 - Iron Deficiency Anemia and Small Bowel Strictures: Thinking Beyond Crohn's Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
