Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0219 - Esophageal Hyperkeratosis Complicated by Recurrent Dysphagia
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Michael Malkowski, MD
St. Elizabeth's Medical Center, Tufts University School of Medicine
Boston, MA
Presenting Author(s)
Michael Malkowski, MD1, Marcel R. Robles, MD2, Aurada Cholapranee, MD1, Aleksandr Perepletchikov, MD, PhD1
1St. Elizabeth's Medical Center, Tufts University School of Medicine, Boston, MA; 2Tufts University School of Medicine, St. Elizabeth's Medical Center, Boston, MA
Introduction: Esophageal hyperkeratosis (EH) is a rare condition characterized by keratinization of the esophageal epithelium. The pathophysiology is poorly understood, and risk factors remain unclear. We present a case of severe long segment EH leading to severe esophageal stenosis.
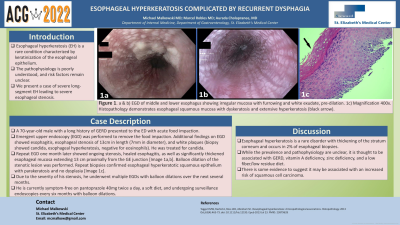
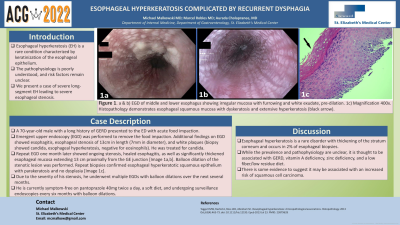
Case Description/Methods: A 70-year-old male with a long history of gastroesophageal reflux disorder (GERD) presented to the ED with acute food impaction. Prior to his presentation, he reported worsening dysphagia and ongoing heartburn for several months. He had been lost to follow-up and was not on any antacids at the time of presentation. Emergent upper endoscopy (EGD) was performed to remove the food impaction. Additional findings on EGD showed esophagitis, esophageal stenosis of 13cm in length (7mm in diameter), and white plaques. Esophageal biopsies were negative for eosinophils but confirmed candida and were suggestive of esophageal hyperkeratosis. Dilation was deferred until the esophagitis was treated with PPI and itraconazole. Repeat EGD one month later showed ongoing stenosis, healed esophagitis, as well as significantly thickened esophageal mucosa extending 13 cm proximally from the GE junction [Image 1a,b]. Balloon dilation of the stenotic lesion was performed. Repeat biopsies confirmed esophageal hyperkeratotic squamous epithelium with parakeratosis and no dysplasia [Image 1c]. Due to the severity of his stenosis, he subsequently underwent multiple EGDs with balloon dilations over the next several months to obtain a maximum esophageal lumen diameter of 19mm. Dilation of his esophagus was particularly difficult due to the length of hyperkeratosis, degree of stenosis, and loss of elasticity of his esophageal mucosa. Tearing of the tissue and bleeding were common even with small interval increases during each dilation session. In addition, healing of the tissue between sessions often led to a restricturing of his esophagus. He is currently symptom-free on pantoprazole 40mg twice a day, a soft diet, and undergoing surveillance endoscopies every six months with balloon dilations.
Discussion: Esophageal hyperkeratosis is a rare disorder with thickening of the stratum corneum and occurs in 2% of esophageal biopsies. While the prevalence and pathophysiology are unclear, it is thought to be associated with GERD, vitamin A deficiency, zinc deficiency, and a low fiber/low residue diet. There is also some evidence to suggest it may be associated with an increased risk of squamous cell carcinoma.

Disclosures:
Michael Malkowski, MD1, Marcel R. Robles, MD2, Aurada Cholapranee, MD1, Aleksandr Perepletchikov, MD, PhD1. A0219 - Esophageal Hyperkeratosis Complicated by Recurrent Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1St. Elizabeth's Medical Center, Tufts University School of Medicine, Boston, MA; 2Tufts University School of Medicine, St. Elizabeth's Medical Center, Boston, MA
Introduction: Esophageal hyperkeratosis (EH) is a rare condition characterized by keratinization of the esophageal epithelium. The pathophysiology is poorly understood, and risk factors remain unclear. We present a case of severe long segment EH leading to severe esophageal stenosis.
Case Description/Methods: A 70-year-old male with a long history of gastroesophageal reflux disorder (GERD) presented to the ED with acute food impaction. Prior to his presentation, he reported worsening dysphagia and ongoing heartburn for several months. He had been lost to follow-up and was not on any antacids at the time of presentation. Emergent upper endoscopy (EGD) was performed to remove the food impaction. Additional findings on EGD showed esophagitis, esophageal stenosis of 13cm in length (7mm in diameter), and white plaques. Esophageal biopsies were negative for eosinophils but confirmed candida and were suggestive of esophageal hyperkeratosis. Dilation was deferred until the esophagitis was treated with PPI and itraconazole. Repeat EGD one month later showed ongoing stenosis, healed esophagitis, as well as significantly thickened esophageal mucosa extending 13 cm proximally from the GE junction [Image 1a,b]. Balloon dilation of the stenotic lesion was performed. Repeat biopsies confirmed esophageal hyperkeratotic squamous epithelium with parakeratosis and no dysplasia [Image 1c]. Due to the severity of his stenosis, he subsequently underwent multiple EGDs with balloon dilations over the next several months to obtain a maximum esophageal lumen diameter of 19mm. Dilation of his esophagus was particularly difficult due to the length of hyperkeratosis, degree of stenosis, and loss of elasticity of his esophageal mucosa. Tearing of the tissue and bleeding were common even with small interval increases during each dilation session. In addition, healing of the tissue between sessions often led to a restricturing of his esophagus. He is currently symptom-free on pantoprazole 40mg twice a day, a soft diet, and undergoing surveillance endoscopies every six months with balloon dilations.
Discussion: Esophageal hyperkeratosis is a rare disorder with thickening of the stratum corneum and occurs in 2% of esophageal biopsies. While the prevalence and pathophysiology are unclear, it is thought to be associated with GERD, vitamin A deficiency, zinc deficiency, and a low fiber/low residue diet. There is also some evidence to suggest it may be associated with an increased risk of squamous cell carcinoma.

Figure: Figure 1: a and b) EGD of middle and lower esophagus showing irregular mucosa with furrowing and white exudate, pre-dilation. 1c) Magnification 400x. Histopathology demonstrates esophageal squamous mucosa with dyskeratosis and extensive hyperkeratosis (black arrow).
Disclosures:
Michael Malkowski indicated no relevant financial relationships.
Marcel Robles indicated no relevant financial relationships.
Aurada Cholapranee indicated no relevant financial relationships.
Aleksandr Perepletchikov indicated no relevant financial relationships.
Michael Malkowski, MD1, Marcel R. Robles, MD2, Aurada Cholapranee, MD1, Aleksandr Perepletchikov, MD, PhD1. A0219 - Esophageal Hyperkeratosis Complicated by Recurrent Dysphagia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
