Back

Poster Session D - Tuesday Morning
Category: Colon
D0144 - Recurrent or Concurrent Colitis: Immune Checkpoint Inhibitor-Induced Colitis vs CMV Colitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Prabhat Kumar, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Achintya Singh, MD1, Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Hassan M. Shaheen, MD1, Asif Hitawala, MD2, Ashraf Almomani, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2National Institutes of Health, Bethesda, MD
Introduction: Diarrhea is among the most common adverse events associated with pembrolizumab and other immune checkpoint inhibitors (ICIs). The successful treatment of diarrhea depends on the timely and accurate diagnosis of the underlying etiology. We present a case of refractory diarrhea due to coinciding cytomegalovirus (CMV) colitis in a patient who developed pembrolizumab-induced colitis.
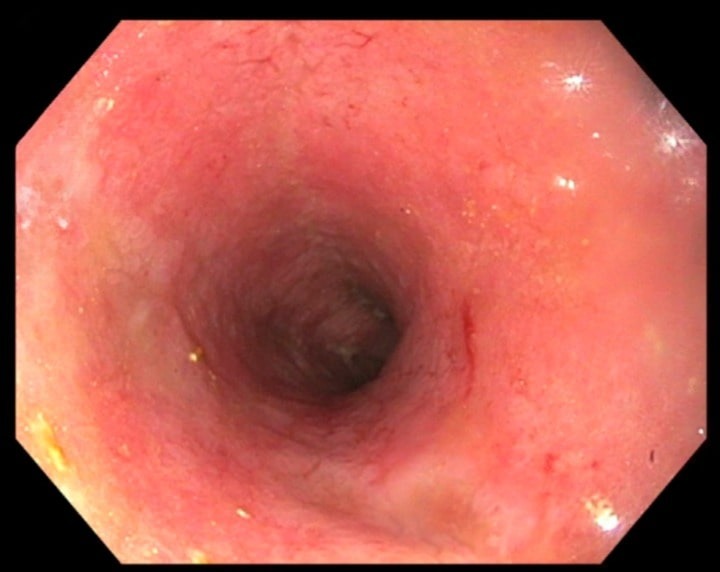
Case Description/Methods: 88-year-old Caucasian male presented to the hospital with chronic diarrhea for three months. He was diagnosed with T4bN0Mx left thigh melanoma, for which he was started on palliative immunotherapy with pembrolizumab one year back. For a year, he tolerated pembrolizumab well without any symptoms until he was hospitalized for ongoing diarrhea for two weeks. His fecal calprotectin was elevated, CMV PCR was undetectable, and CMV immunostaining was negative. Sigmoidoscopy was significant for the congested, erythematous, and inflamed mucosa in the distal sigmoid colon, suggesting acute colitis (figure). This was assumed to be pembrolizumab related to colitis, and he was discharged on a prednisone taper. However, he continued to have diarrhea, and a couple of months later, he was readmitted for similar complaints. An extensive infectious disease workup was done to rule out other causes of chronic diarrhea. CMV DNA was detected by PCR ( >5000 copies/mL), although histopathological studies were negative for CMV inclusions. Our patient was started on valganciclovir infusion for two weeks and received symptomatic management and anti-diarrheal agents. Repeat CMV titers trended down, and his diarrhea improved.
Discussion: Treatment with ICIs is often associated with transient but occasionally severe colitis. The diagnosis of ICI diarrhea requires thorough testing to rule out infectious and other inflammatory causes of colitis; an endoscopic biopsy is ultimately needed to make the diagnosis. Interruption of the ICI and systemic immunosuppression with corticosteroids optimizes outcome in most patients. On the other hand, corticosteroid immunosuppression can lead to activation of CMV, manifesting as transient improvement and then worsening to refractory diarrhea. Repeat infectious workup and endoscopic re-evaluation with tissue biopsy are needed to confirm the diagnosis of CMV colitis. Prompt discontinuation of corticosteroids and initiation of antivirals leads to spontaneous resolution of symptoms.
Disclosures:
Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Achintya Singh, MD1, Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Hassan M. Shaheen, MD1, Asif Hitawala, MD2, Ashraf Almomani, MD1. D0144 - Recurrent or Concurrent Colitis: Immune Checkpoint Inhibitor-Induced Colitis vs CMV Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2National Institutes of Health, Bethesda, MD
Introduction: Diarrhea is among the most common adverse events associated with pembrolizumab and other immune checkpoint inhibitors (ICIs). The successful treatment of diarrhea depends on the timely and accurate diagnosis of the underlying etiology. We present a case of refractory diarrhea due to coinciding cytomegalovirus (CMV) colitis in a patient who developed pembrolizumab-induced colitis.
Case Description/Methods: 88-year-old Caucasian male presented to the hospital with chronic diarrhea for three months. He was diagnosed with T4bN0Mx left thigh melanoma, for which he was started on palliative immunotherapy with pembrolizumab one year back. For a year, he tolerated pembrolizumab well without any symptoms until he was hospitalized for ongoing diarrhea for two weeks. His fecal calprotectin was elevated, CMV PCR was undetectable, and CMV immunostaining was negative. Sigmoidoscopy was significant for the congested, erythematous, and inflamed mucosa in the distal sigmoid colon, suggesting acute colitis (figure). This was assumed to be pembrolizumab related to colitis, and he was discharged on a prednisone taper. However, he continued to have diarrhea, and a couple of months later, he was readmitted for similar complaints. An extensive infectious disease workup was done to rule out other causes of chronic diarrhea. CMV DNA was detected by PCR ( >5000 copies/mL), although histopathological studies were negative for CMV inclusions. Our patient was started on valganciclovir infusion for two weeks and received symptomatic management and anti-diarrheal agents. Repeat CMV titers trended down, and his diarrhea improved.
Discussion: Treatment with ICIs is often associated with transient but occasionally severe colitis. The diagnosis of ICI diarrhea requires thorough testing to rule out infectious and other inflammatory causes of colitis; an endoscopic biopsy is ultimately needed to make the diagnosis. Interruption of the ICI and systemic immunosuppression with corticosteroids optimizes outcome in most patients. On the other hand, corticosteroid immunosuppression can lead to activation of CMV, manifesting as transient improvement and then worsening to refractory diarrhea. Repeat infectious workup and endoscopic re-evaluation with tissue biopsy are needed to confirm the diagnosis of CMV colitis. Prompt discontinuation of corticosteroids and initiation of antivirals leads to spontaneous resolution of symptoms.
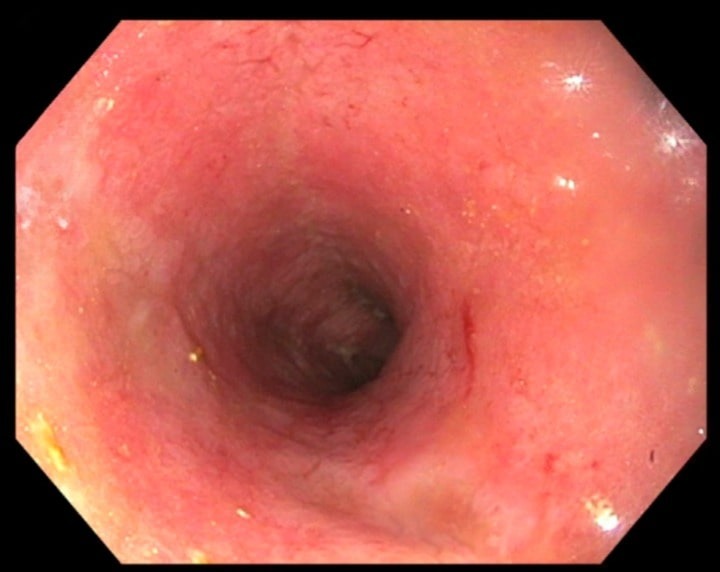
Figure: Colonoscopy showing the diffuse area of moderately congested, erythematous, and inflamed mucosa in the distal sigmoid colon.
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Achintya Singh indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Eduard Krishtopaytis indicated no relevant financial relationships.
Hassan Shaheen indicated no relevant financial relationships.
Asif Hitawala indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Prabhat Kumar, MD1, Somtochukwu Onwuzo, MD1, Achintya Singh, MD1, Antoine Boustany, MD, MPH1, Eduard Krishtopaytis, MD1, Hassan M. Shaheen, MD1, Asif Hitawala, MD2, Ashraf Almomani, MD1. D0144 - Recurrent or Concurrent Colitis: Immune Checkpoint Inhibitor-Induced Colitis vs CMV Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
