Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0323 - A Case of Spontaneous Duodenocaval Fistula Formation in a Patient With a Large Necrotic Duodenal Ulcer
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Malek Kreidieh, MD
Staten Island University Hospital
Staten Island, NY
Presenting Author(s)
Malek Kreidieh, MD, Shivantha Amarnath, MD, Dhineshreddy Gurala, MD, Stephen Mulrooney, MD
Staten Island University Hospital, Staten Island, NY
Introduction: Duodenocaval fistulas (DCFs) are rare digestive fistulas that present with gastrointestinal bleeding and sepsis and carry a 40% mortality rate. Most reported cases usually have a predisposing event, including a penetrating abdominal trauma, a penetrating strut of a retrievable inferior vena cava (IVC) filter, or a foreign body impaction in the duodenum. A few cases have been reported in patients with no prior trauma or surgery, such as those with a history of peptic ulcer disease (PUD). We present a rare case of spontaneous DCF formation in a patient with a history of a PUD who presented with fresh, bright red blood per rectum (FBRBR) and sepsis secondary to bacteremia and fungemia.
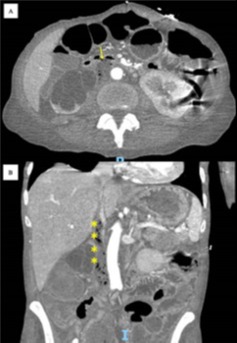
Case Description/Methods: A 63-year-old female patient with a history of a 3cm necrotic ulcer in the second part of the duodenum and stage III ovarian cancer status post total abdominal hysterectomy on active chemoradiotherapy, with the last session being a month prior to presentation, presented for evaluation of a 5-day history of FBRBR with clots in the setting of recent excessive non-steroidal anti-inflammatory drugs (NSAIDs) use. On presentation, the patient was hypotensive and tachycardic. The initial investigation was notable for an acute drop in hemoglobin from a baseline of 8.7g/dL to 3.6 g/dL and an acute kidney injury. The patient received empiric intravenous antibiotics, intravenous fluid boluses, and six units of packed red blood cells with an improvement in vital signs and hemoglobin. Blood cultures grew Enterococcus Faecalis, Streptococcus anginosus, and Candida albicans. A computed tomography angiography (CTA) of the abdomen and pelvis with intravenous contrast was performed, revealing evidence of locules of gas within the intrahepatic IVC with communication with the duodenal lumen suggestive of a duodenocaval fistula (Fig. 1). The interventional radiology team was consulted and recommended surgical evaluation as the case was not amenable to endovascular intervention. General surgery, surgical oncology, and vascular teams concluded that intraoperative mortality associated with reconstruction would approach 100%. The patient was then evaluated by palliative and hospice teams, and she was discharged with home hospice services two days after admission.
Discussion: Our case emphasizes that in patients presenting with FBRBR and sepsis, clinicians should have a high suspicion of DCFs, especially in the setting of a history of PUD, abdominal surgery and radiotherapy, and recent excessive NSAID use.
Disclosures:
Malek Kreidieh, MD, Shivantha Amarnath, MD, Dhineshreddy Gurala, MD, Stephen Mulrooney, MD. D0323 - A Case of Spontaneous Duodenocaval Fistula Formation in a Patient With a Large Necrotic Duodenal Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Staten Island University Hospital, Staten Island, NY
Introduction: Duodenocaval fistulas (DCFs) are rare digestive fistulas that present with gastrointestinal bleeding and sepsis and carry a 40% mortality rate. Most reported cases usually have a predisposing event, including a penetrating abdominal trauma, a penetrating strut of a retrievable inferior vena cava (IVC) filter, or a foreign body impaction in the duodenum. A few cases have been reported in patients with no prior trauma or surgery, such as those with a history of peptic ulcer disease (PUD). We present a rare case of spontaneous DCF formation in a patient with a history of a PUD who presented with fresh, bright red blood per rectum (FBRBR) and sepsis secondary to bacteremia and fungemia.
Case Description/Methods: A 63-year-old female patient with a history of a 3cm necrotic ulcer in the second part of the duodenum and stage III ovarian cancer status post total abdominal hysterectomy on active chemoradiotherapy, with the last session being a month prior to presentation, presented for evaluation of a 5-day history of FBRBR with clots in the setting of recent excessive non-steroidal anti-inflammatory drugs (NSAIDs) use. On presentation, the patient was hypotensive and tachycardic. The initial investigation was notable for an acute drop in hemoglobin from a baseline of 8.7g/dL to 3.6 g/dL and an acute kidney injury. The patient received empiric intravenous antibiotics, intravenous fluid boluses, and six units of packed red blood cells with an improvement in vital signs and hemoglobin. Blood cultures grew Enterococcus Faecalis, Streptococcus anginosus, and Candida albicans. A computed tomography angiography (CTA) of the abdomen and pelvis with intravenous contrast was performed, revealing evidence of locules of gas within the intrahepatic IVC with communication with the duodenal lumen suggestive of a duodenocaval fistula (Fig. 1). The interventional radiology team was consulted and recommended surgical evaluation as the case was not amenable to endovascular intervention. General surgery, surgical oncology, and vascular teams concluded that intraoperative mortality associated with reconstruction would approach 100%. The patient was then evaluated by palliative and hospice teams, and she was discharged with home hospice services two days after admission.
Discussion: Our case emphasizes that in patients presenting with FBRBR and sepsis, clinicians should have a high suspicion of DCFs, especially in the setting of a history of PUD, abdominal surgery and radiotherapy, and recent excessive NSAID use.
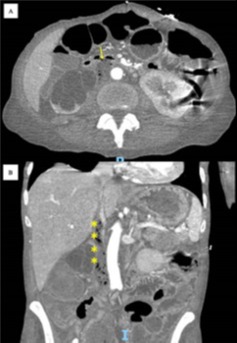
Figure: Figure 1. Axial (A) and coronal (B) views of an enhanced abdominal CTA scan demonstrating locules of gas within the inferior vena cava (yellow asterixis) with communication with the duodenal lumen (yellow arrow) suggestive of a duodenocaval fistula.
Disclosures:
Malek Kreidieh indicated no relevant financial relationships.
Shivantha Amarnath indicated no relevant financial relationships.
Dhineshreddy Gurala indicated no relevant financial relationships.
Stephen Mulrooney indicated no relevant financial relationships.
Malek Kreidieh, MD, Shivantha Amarnath, MD, Dhineshreddy Gurala, MD, Stephen Mulrooney, MD. D0323 - A Case of Spontaneous Duodenocaval Fistula Formation in a Patient With a Large Necrotic Duodenal Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

