Back

Poster Session A - Sunday Afternoon
Category: Liver
A0565 - Bleeding IGV2 from Left-Sided Portal Hypertension in a Decompensated Cirrhotic
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- CS
Chad Spencer, MD
University of South Alabama
Mobile, AL
Presenting Author(s)
Chad Spencer, MD, Phillip Henderson, DO
University of South Alabama, Mobile, AL
Introduction: Variceal hemorrhage is one of the leading causes of morbidity and mortality in cirrhosis. While esophageal varices (EVs) are more likely to bleed, bleeding from gastric varices is typically more severe and carries higher mortality. IGV2, isolated gastric varices located outside of the cardiofundal region, are very rarely seen in patients with cirrhosis and do not frequently result in bleeding. Here we discuss a complex case of bleeding IGV2 in a cirrhotic patient who developed left-sided portal hypertension due to splenic vein thrombosis.
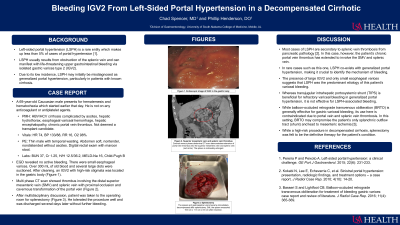
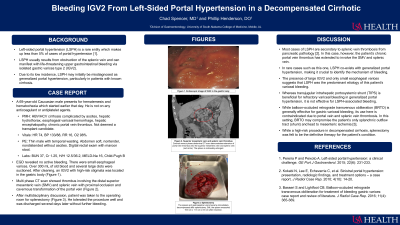
Case Description/Methods: A 69-year-old white male with decompensated Child-Pugh B cirrhosis presented with acute onset hematemesis and hematochezia. He has a known chronic portal vein thrombus for which he was not anticoagulated, as he was not deemed a liver transplant candidate. Initial vitals were in normal range. Initial labs were notable for hemoglobin 12.5 g/dL, blood urea nitrogen 37 mg/dL, and MELD-Na 16. He was administered octreotide and ceftriaxone and taken for upper endoscopy. Upper endoscopy revealed small, nonbleeding EVs and copious gastric blood. Large IGV2 with stigmata of recent bleeding were identified in the gastric body. Multiphasic computed tomography showed several portosystemic shunts, cavernous transformation of the portal vein, and thrombus extending into the superior mesenteric vein (SMV) and splenic vein. After multidisciplinary discussion, the patient was taken for splenectomy which resulted in variceal decompression. Hepatic function remained at baseline following surgery and bleeding did not recur.
Discussion: This case highlights the multidisciplinary and collaborative approach which is required for management of bleeding IGV2. Ultimately, approach depends on the patient’s vascular anatomy, which in cases of cirrhosis may be quite complex due to portosystemic shunts and collateral vessels. As such, diagnostic radiology, interventional radiology, gastroenterology, and surgery were all involved in this case. While transjugular intrahepatic portosystemic shunt (TIPS) and balloon occluded retrograde transvenous obliteration (BRTO) play big roles in managing most gastric varices, TIPS would not have decompressed the left side of the portal system due to thrombus. BRTO, while perhaps more efficacious, would carry risk of intestinal ischemia in the setting of SMV thrombus, as occlusion of collateral vessels may disrupt drainage of the small bowel. Splenectomy was therefore felt to be the most definitive management.
Disclosures:
Chad Spencer, MD, Phillip Henderson, DO. A0565 - Bleeding IGV2 from Left-Sided Portal Hypertension in a Decompensated Cirrhotic, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of South Alabama, Mobile, AL
Introduction: Variceal hemorrhage is one of the leading causes of morbidity and mortality in cirrhosis. While esophageal varices (EVs) are more likely to bleed, bleeding from gastric varices is typically more severe and carries higher mortality. IGV2, isolated gastric varices located outside of the cardiofundal region, are very rarely seen in patients with cirrhosis and do not frequently result in bleeding. Here we discuss a complex case of bleeding IGV2 in a cirrhotic patient who developed left-sided portal hypertension due to splenic vein thrombosis.
Case Description/Methods: A 69-year-old white male with decompensated Child-Pugh B cirrhosis presented with acute onset hematemesis and hematochezia. He has a known chronic portal vein thrombus for which he was not anticoagulated, as he was not deemed a liver transplant candidate. Initial vitals were in normal range. Initial labs were notable for hemoglobin 12.5 g/dL, blood urea nitrogen 37 mg/dL, and MELD-Na 16. He was administered octreotide and ceftriaxone and taken for upper endoscopy. Upper endoscopy revealed small, nonbleeding EVs and copious gastric blood. Large IGV2 with stigmata of recent bleeding were identified in the gastric body. Multiphasic computed tomography showed several portosystemic shunts, cavernous transformation of the portal vein, and thrombus extending into the superior mesenteric vein (SMV) and splenic vein. After multidisciplinary discussion, the patient was taken for splenectomy which resulted in variceal decompression. Hepatic function remained at baseline following surgery and bleeding did not recur.
Discussion: This case highlights the multidisciplinary and collaborative approach which is required for management of bleeding IGV2. Ultimately, approach depends on the patient’s vascular anatomy, which in cases of cirrhosis may be quite complex due to portosystemic shunts and collateral vessels. As such, diagnostic radiology, interventional radiology, gastroenterology, and surgery were all involved in this case. While transjugular intrahepatic portosystemic shunt (TIPS) and balloon occluded retrograde transvenous obliteration (BRTO) play big roles in managing most gastric varices, TIPS would not have decompressed the left side of the portal system due to thrombus. BRTO, while perhaps more efficacious, would carry risk of intestinal ischemia in the setting of SMV thrombus, as occlusion of collateral vessels may disrupt drainage of the small bowel. Splenectomy was therefore felt to be the most definitive management.
Disclosures:
Chad Spencer indicated no relevant financial relationships.
Phillip Henderson indicated no relevant financial relationships.
Chad Spencer, MD, Phillip Henderson, DO. A0565 - Bleeding IGV2 from Left-Sided Portal Hypertension in a Decompensated Cirrhotic, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

