Back

Poster Session E - Tuesday Afternoon
Category: Biliary/Pancreas
E0071 - Metastatic Solid Pseudopapillary Neoplasm of the Pancreas, Rare Presentation of an Uncommon Tumor
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Kelli C. Kosako Yost, MD
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Kelli C. Kosako Yost, MD1, Paul Gomez, MD1, Shivakumar Vignesh, MD2, Hiba Ibrahim, MD3, Rajesh Ramanathan, MD4
1University of Arizona College of Medicine, Phoenix, AZ; 2Banner MD Anderson Cancer Center at Banner University Medical Center, Phoenix, AZ; 3Clin-Path Associates PLC, Phoenix, AZ; 4Banner MD Anderson Cancer Center, Gilbert, AZ
Introduction: Solid pseudopapillary neoplasms (SPN) make up less than 3% of all diagnosed pancreatic neoplasms. Abdominal CT or MRI are the imaging modalities most utilized, and biopsy is necessary to confirm the diagnosis. Resection of the mass is standard of care and the prognosis is quite good, with 5-year survival rates of over 95%. Both recurrence and metastasis of the tumor are exceedingly rare, occurring in only 1-4% of patients.
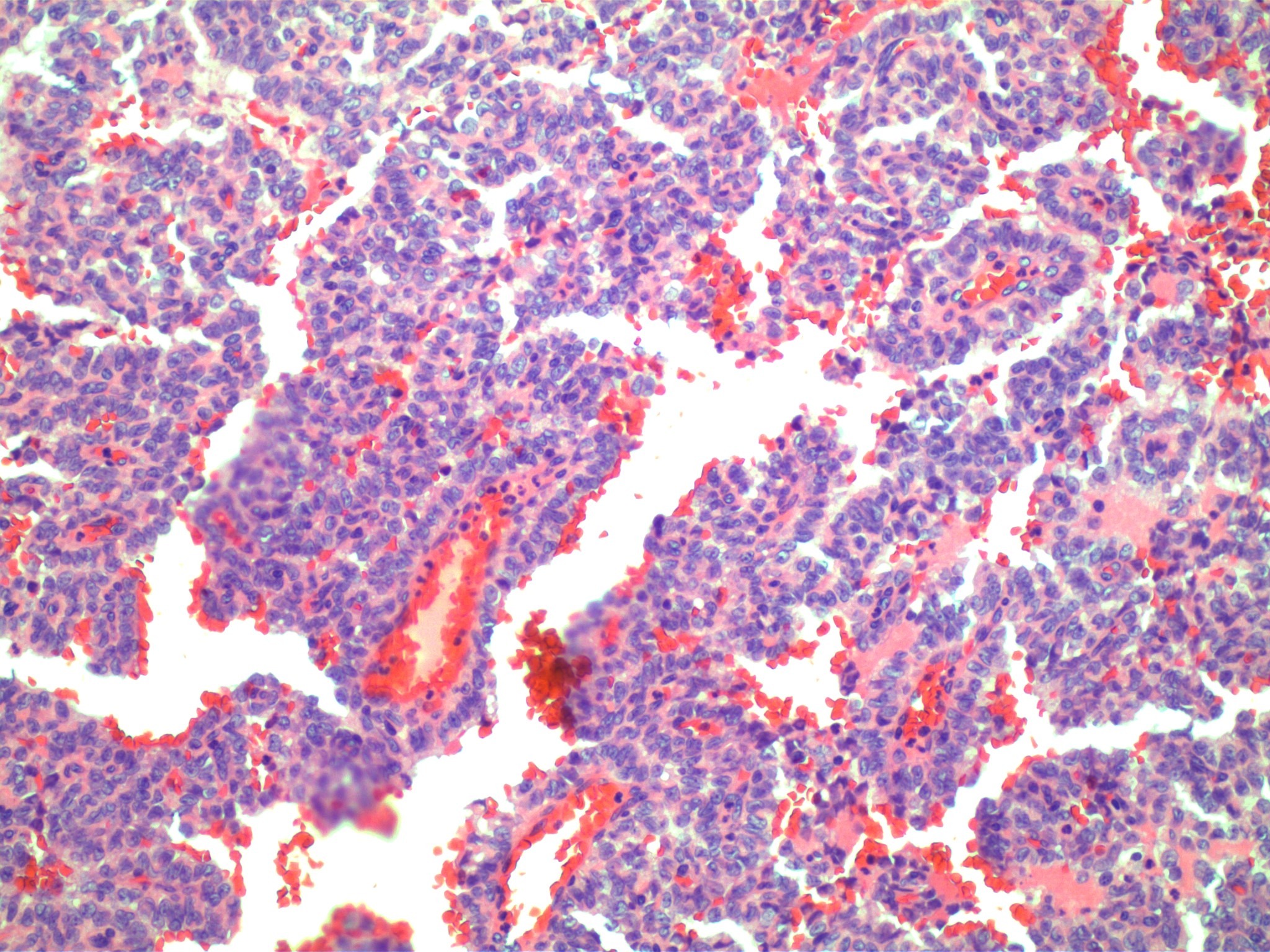
Case Description/Methods: A 26-year-old female presented with several years of abdominal pain. CT scan revealed a 10cm mass in the neck and body of the pancreas and patient underwent a hybrid resection including subtotal pancreatectomy, splenectomy, and cholecystectomy. Pathology showed a neoplasm extending to the inked margins with positive beta-catenin and CD10 nuclear staining with no evidence of metastasis. At the age of 32, the patient presented again with abdominal pain. A CT and PET scan showed numerous LUQ, perirenal, pancreatic, and periadrenal soft tissue densities. Laparoscopic resection of a 3.5x3 cm soft tissue mass near the remnant pancreas was performed, showing fibrous stroma with angulated islands of epithelioid cells with cystic degeneration and positive staining for vimentin, CD56, and beta-catenin. Resection of multiple abdominal soft tissue tumors, in bulk measuring more than 10 cm, as well as complete omentectomy, left adrenalectomy, bilateral salpingo-oophorectomy, appendectomy, and hyperthermic intraperitoneal chemotherapy with cisplatin was performed. Pathology showed multiple metastatic tumors all consistent with SPN. The appendix, left adrenal gland, bilateral ovaries, and all lymph nodes were negative for any tumor. Two years later, MRI revealed 3.0 x 2.1 cm hyperintense lesion in the caudate lobe of the liver. EUS with biopsy was performed, revealing clusters of uniform, bland cells with ovoid nuclei and associated fibrillary stroma circumscribing vessels with a background of hemorrhagic debris (Figure 1). Immunohistochemistry showed cells positive for vimentin, LEF1, and beta-catenin, again consistent with SPN.
Discussion: This is one of the few cases of multiple instances of both recurrence and metastasis of SPN documented in the literature. This case report shows that serial imaging studies and close follow-up are needed even years after resection and that, although rare, recurrence and metastasis can occur more than one time after the initial diagnosis.
Disclosures:
Kelli C. Kosako Yost, MD1, Paul Gomez, MD1, Shivakumar Vignesh, MD2, Hiba Ibrahim, MD3, Rajesh Ramanathan, MD4. E0071 - Metastatic Solid Pseudopapillary Neoplasm of the Pancreas, Rare Presentation of an Uncommon Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Arizona College of Medicine, Phoenix, AZ; 2Banner MD Anderson Cancer Center at Banner University Medical Center, Phoenix, AZ; 3Clin-Path Associates PLC, Phoenix, AZ; 4Banner MD Anderson Cancer Center, Gilbert, AZ
Introduction: Solid pseudopapillary neoplasms (SPN) make up less than 3% of all diagnosed pancreatic neoplasms. Abdominal CT or MRI are the imaging modalities most utilized, and biopsy is necessary to confirm the diagnosis. Resection of the mass is standard of care and the prognosis is quite good, with 5-year survival rates of over 95%. Both recurrence and metastasis of the tumor are exceedingly rare, occurring in only 1-4% of patients.
Case Description/Methods: A 26-year-old female presented with several years of abdominal pain. CT scan revealed a 10cm mass in the neck and body of the pancreas and patient underwent a hybrid resection including subtotal pancreatectomy, splenectomy, and cholecystectomy. Pathology showed a neoplasm extending to the inked margins with positive beta-catenin and CD10 nuclear staining with no evidence of metastasis. At the age of 32, the patient presented again with abdominal pain. A CT and PET scan showed numerous LUQ, perirenal, pancreatic, and periadrenal soft tissue densities. Laparoscopic resection of a 3.5x3 cm soft tissue mass near the remnant pancreas was performed, showing fibrous stroma with angulated islands of epithelioid cells with cystic degeneration and positive staining for vimentin, CD56, and beta-catenin. Resection of multiple abdominal soft tissue tumors, in bulk measuring more than 10 cm, as well as complete omentectomy, left adrenalectomy, bilateral salpingo-oophorectomy, appendectomy, and hyperthermic intraperitoneal chemotherapy with cisplatin was performed. Pathology showed multiple metastatic tumors all consistent with SPN. The appendix, left adrenal gland, bilateral ovaries, and all lymph nodes were negative for any tumor. Two years later, MRI revealed 3.0 x 2.1 cm hyperintense lesion in the caudate lobe of the liver. EUS with biopsy was performed, revealing clusters of uniform, bland cells with ovoid nuclei and associated fibrillary stroma circumscribing vessels with a background of hemorrhagic debris (Figure 1). Immunohistochemistry showed cells positive for vimentin, LEF1, and beta-catenin, again consistent with SPN.
Discussion: This is one of the few cases of multiple instances of both recurrence and metastasis of SPN documented in the literature. This case report shows that serial imaging studies and close follow-up are needed even years after resection and that, although rare, recurrence and metastasis can occur more than one time after the initial diagnosis.
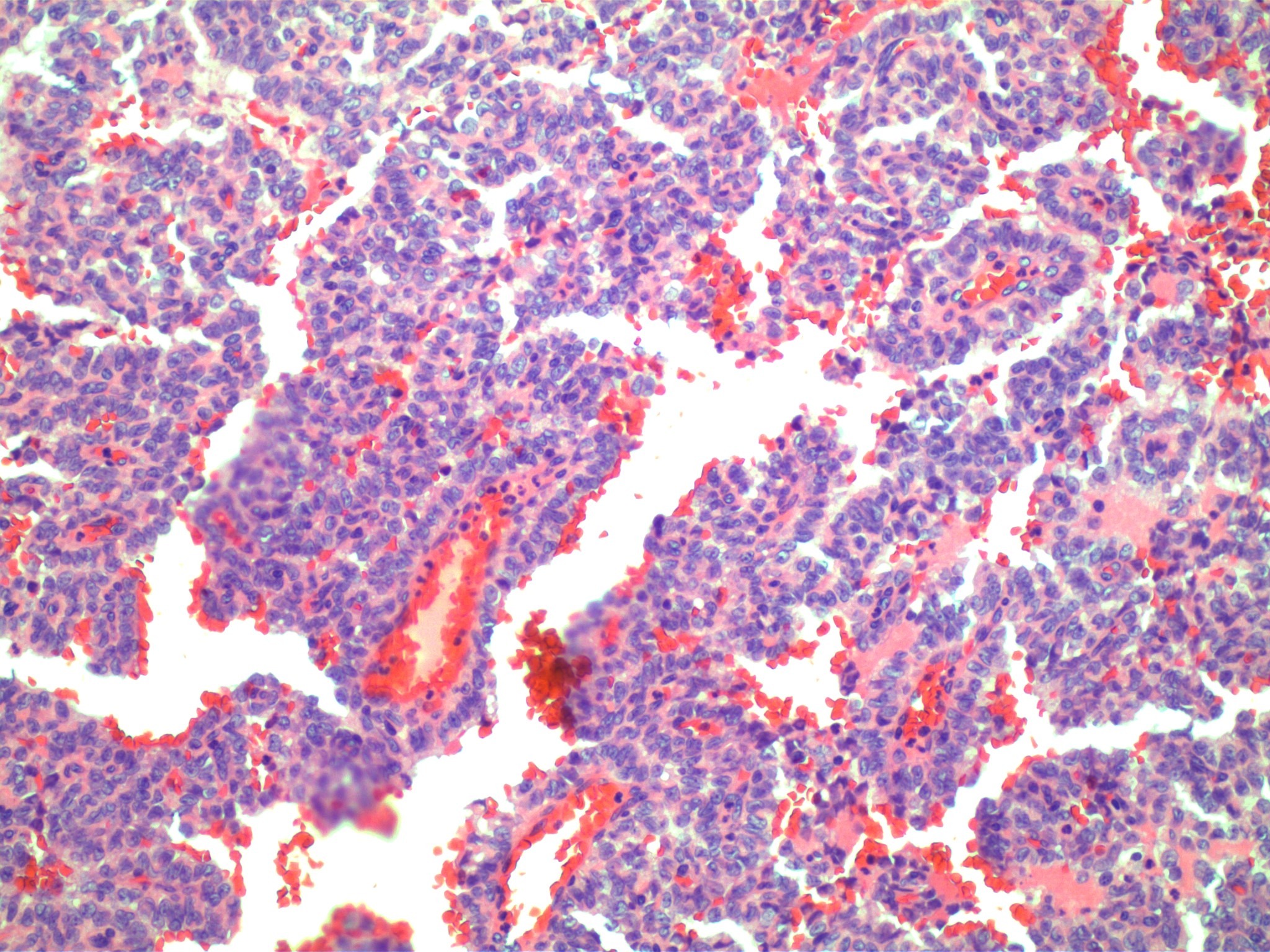
Figure: Figure 1: Biopsy of the caudate liver lesion showing clusters of uniform, bland cells with ovoid nuclei and associated fibrillary stroma and hemorrhagic debris, consistent with SPN
Disclosures:
Kelli Kosako Yost indicated no relevant financial relationships.
Paul Gomez indicated no relevant financial relationships.
Shivakumar Vignesh indicated no relevant financial relationships.
Hiba Ibrahim indicated no relevant financial relationships.
Rajesh Ramanathan indicated no relevant financial relationships.
Kelli C. Kosako Yost, MD1, Paul Gomez, MD1, Shivakumar Vignesh, MD2, Hiba Ibrahim, MD3, Rajesh Ramanathan, MD4. E0071 - Metastatic Solid Pseudopapillary Neoplasm of the Pancreas, Rare Presentation of an Uncommon Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

