Back


Poster Session A - Sunday Afternoon
Category: Interventional Endoscopy
A0447 - Biliary Stenting of Caustic Proximal Esophageal Stricture Complicated by Fistula From Prior Dilation
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Has Audio

Mohamad I. Itani, MD
Wayne State University / Detroit Medical Center
Detroit, MI
Presenting Author(s)
Mohamad I. Itani, MD1, Anirudh R. Damughatla, DO2, Baraa Osman, DO1, Ahmad Abu-Heija, MBBS1, Lawrence N. Diebel, MD3, Thomas E. Kelly, MD3
1Wayne State University / Detroit Medical Center, Detroit, MI; 2Wayne State University/Detroit Medical Center, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI
Introduction: Caustic ingestions can lead to recalcitrant strictures of the upper esophagus. Endoscopic treatment options include dilations and/or covered esophageal stents; however, a stricture at a high anatomic location renders traditional stenting difficult. Dilation has the risk of perforation and fistula development. We present a patient with complex, proximal and distal esophageal strictures from caustic ingestion who was managed surgically then salvaged endoscopically using biliary stents.
Case Description/Methods: A 28-year-old woman with a history of caustic ingestion of bleach and was found to have airway injuries, severe proximal digestive tract injuries, and transmural gastric necrosis. She underwent a total gastrectomy and cervical esophagostomy followed by Roux esophagojejunostomy and stepwise reconstruction. She then had esophageal strictures initially treated with Savary dilation complicated by perforation and fistula formation between upper stricture and pleura.
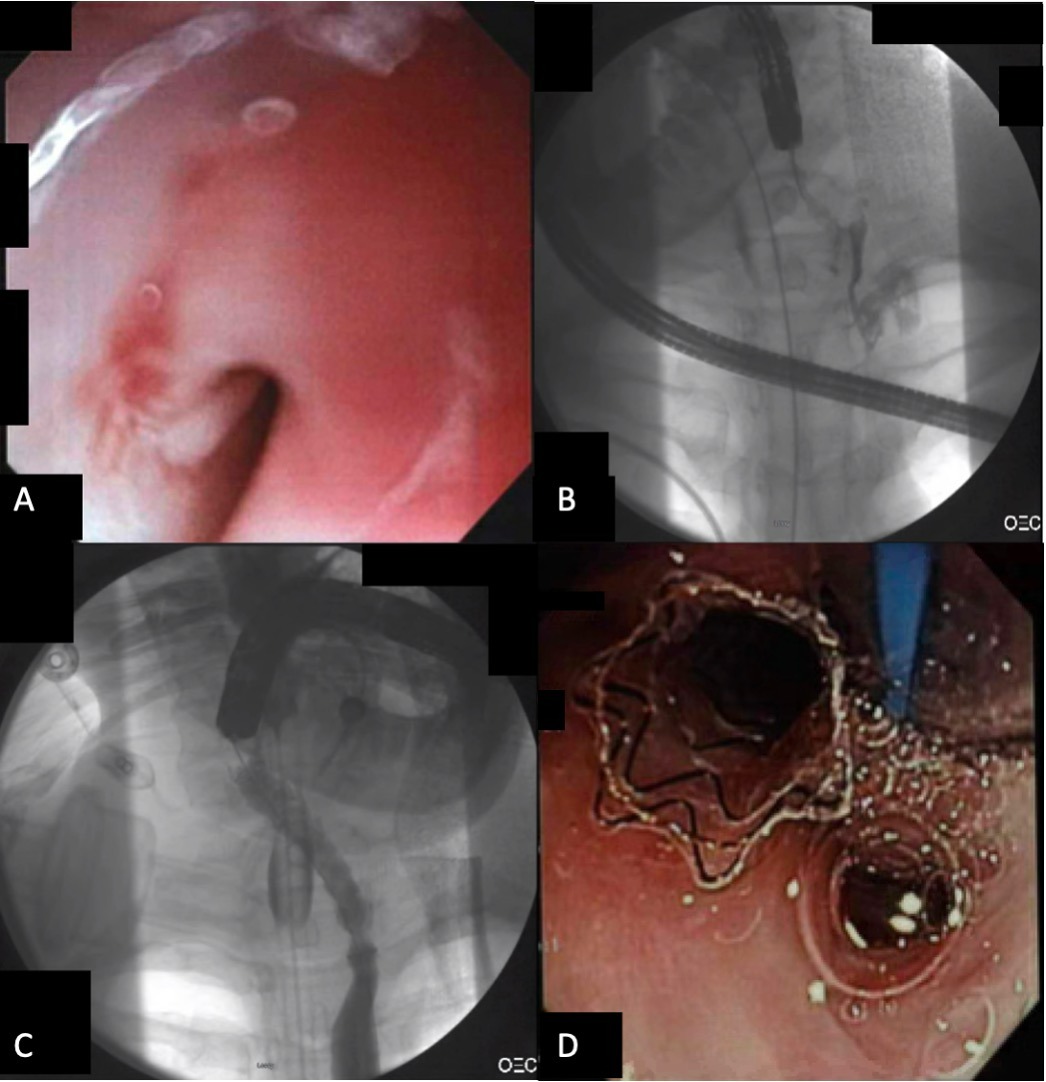
Endoscopy revealed a 3-mm lumen at the upper esophageal sphincter (UES)(Figure 1). Initial contrast injection revealed no passage into esophagus, with contrast passing to pleura. XP gastroscope was used to pass a guidewire through the proximal stricture and into the esophagus. A 10mm x 6cm biliary fully covered self-expanding metal stent (FCSEMS; Gore Viabil Biliary Endoprosthesis) was deployed across the stricture, covering the fistula. The patient subsequently had repeated endoscopies for stent migration and to reach the distal stricture for stenting.
Discussion: Esophageal stents are not typically placed across the UES due to foreign body sensation. In this case, the anatomic location of the stricture and presence of fistula required stenting across the UES. We chose a biliary FCSEMS that had anti-migratory features (flanges and conformability) and did not foreshorten. Despite these measures, the stent did migrate multiple times requiring re-intervention over a period of months, eventually allowing access to the distal esophageal stricture after upper esophageal remodeling around the shape of the stent. At the time of presentation to advanced endoscopy, colonic interposition was a less preferred option due to lack of healthy pharyngeal or esophageal tissue for anastomosis. Through the use of biliary stents in the esophagus, we were able to simultaneously treat a difficult stricture and fistula, allowing eventual access to a distal stricture for endoscopic treatment.
Disclosures:
Mohamad I. Itani, MD1, Anirudh R. Damughatla, DO2, Baraa Osman, DO1, Ahmad Abu-Heija, MBBS1, Lawrence N. Diebel, MD3, Thomas E. Kelly, MD3. A0447 - Biliary Stenting of Caustic Proximal Esophageal Stricture Complicated by Fistula From Prior Dilation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wayne State University / Detroit Medical Center, Detroit, MI; 2Wayne State University/Detroit Medical Center, Detroit, MI; 3Wayne State University School of Medicine, Detroit, MI
Introduction: Caustic ingestions can lead to recalcitrant strictures of the upper esophagus. Endoscopic treatment options include dilations and/or covered esophageal stents; however, a stricture at a high anatomic location renders traditional stenting difficult. Dilation has the risk of perforation and fistula development. We present a patient with complex, proximal and distal esophageal strictures from caustic ingestion who was managed surgically then salvaged endoscopically using biliary stents.
Case Description/Methods: A 28-year-old woman with a history of caustic ingestion of bleach and was found to have airway injuries, severe proximal digestive tract injuries, and transmural gastric necrosis. She underwent a total gastrectomy and cervical esophagostomy followed by Roux esophagojejunostomy and stepwise reconstruction. She then had esophageal strictures initially treated with Savary dilation complicated by perforation and fistula formation between upper stricture and pleura.
Endoscopy revealed a 3-mm lumen at the upper esophageal sphincter (UES)(Figure 1). Initial contrast injection revealed no passage into esophagus, with contrast passing to pleura. XP gastroscope was used to pass a guidewire through the proximal stricture and into the esophagus. A 10mm x 6cm biliary fully covered self-expanding metal stent (FCSEMS; Gore Viabil Biliary Endoprosthesis) was deployed across the stricture, covering the fistula. The patient subsequently had repeated endoscopies for stent migration and to reach the distal stricture for stenting.
Discussion: Esophageal stents are not typically placed across the UES due to foreign body sensation. In this case, the anatomic location of the stricture and presence of fistula required stenting across the UES. We chose a biliary FCSEMS that had anti-migratory features (flanges and conformability) and did not foreshorten. Despite these measures, the stent did migrate multiple times requiring re-intervention over a period of months, eventually allowing access to the distal esophageal stricture after upper esophageal remodeling around the shape of the stent. At the time of presentation to advanced endoscopy, colonic interposition was a less preferred option due to lack of healthy pharyngeal or esophageal tissue for anastomosis. Through the use of biliary stents in the esophagus, we were able to simultaneously treat a difficult stricture and fistula, allowing eventual access to a distal stricture for endoscopic treatment.
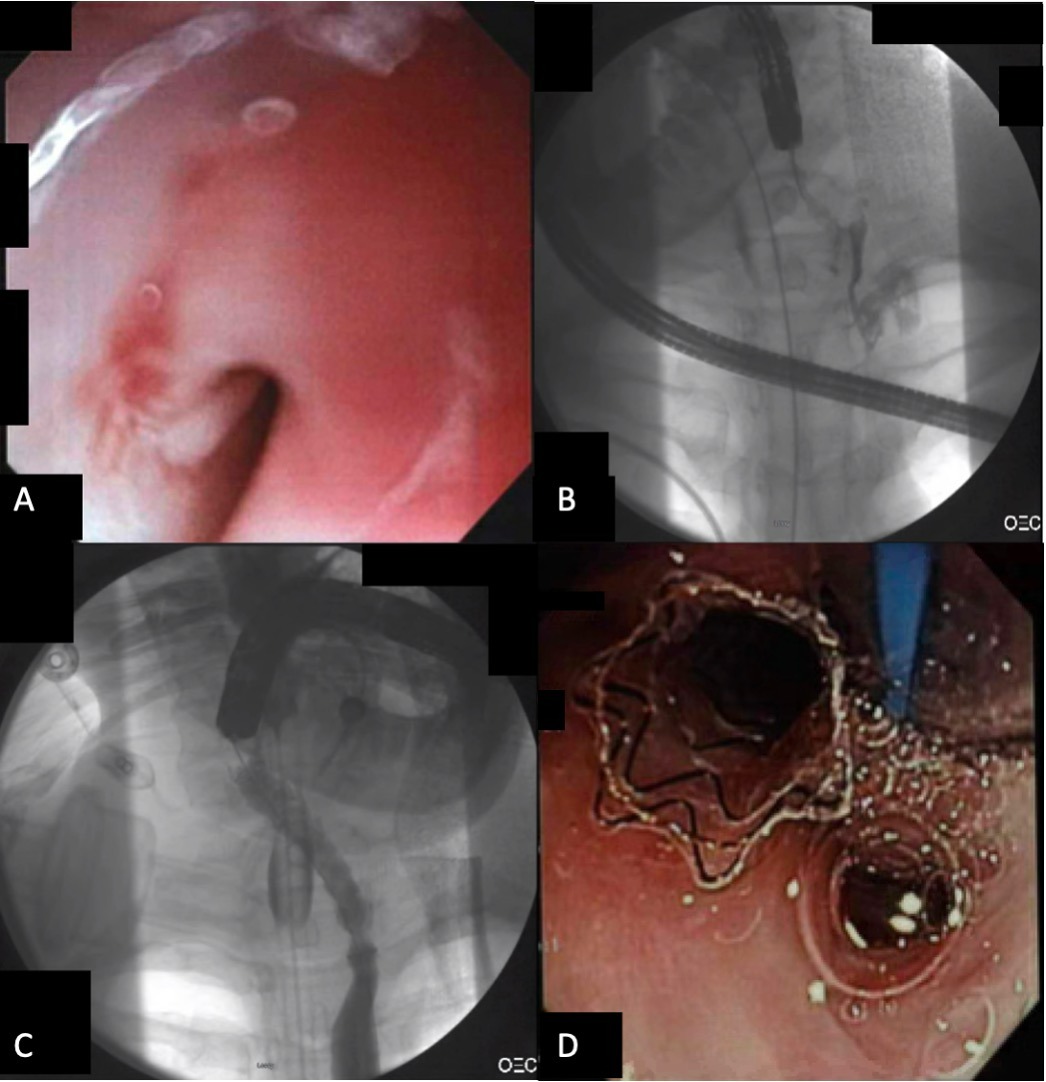
Figure: Figure 1: Endoscopic and fluoroscopic imaging showing (A) proximal esophageal stricture from caustic ingestion, (B) contrast injection showing stricture with fistula to pleura prior to stenting, (C) contrast injection through biliary FCSEMS deployed across proximal stricture without evidence of leak, and (D) proximal endoscopic view of the biliary FCSEMS above the arytenoid and close to endotracheal tube in subsequent endoscopy.
Disclosures:
Mohamad I. Itani indicated no relevant financial relationships.
Anirudh Damughatla indicated no relevant financial relationships.
Baraa Osman indicated no relevant financial relationships.
Ahmad Abu-Heija indicated no relevant financial relationships.
Lawrence Diebel indicated no relevant financial relationships.
Thomas E. Kelly indicated no relevant financial relationships.
Mohamad I. Itani, MD1, Anirudh R. Damughatla, DO2, Baraa Osman, DO1, Ahmad Abu-Heija, MBBS1, Lawrence N. Diebel, MD3, Thomas E. Kelly, MD3. A0447 - Biliary Stenting of Caustic Proximal Esophageal Stricture Complicated by Fistula From Prior Dilation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
