Back

Poster Session D - Tuesday Morning
Category: Interventional Endoscopy
D0461 - Migrated Esophageal Stent Obstructing the Distal Jejunum, Safely Removed by Double-Balloon Enteroscopy Using a Water Immersion Technique
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- OS
Otis Stephen, MD
Cedars Sinai Medical Center
Los Angeles, CA
Presenting Author(s)
Otis Stephen, MD
Cedars Sinai Medical Center, Los Angeles, CA
Introduction: Self-expanding esophageal metal stents are now also used for treatment of gastric and duodenal lesions. Stent migration is a potential risk. Endoscopic retrieval after distal small bowel migration is challenging, often requiring surgery. Double-Balloon Enteroscopy (DBE) enables endoscopic access throughout the small bowel, but small bowel tortuosity makes retrieval of stents in the distal small bowel extremely challenging, so it is performed infrequently.
We describe a case of migration of a fully covered metal stent to the distal jejunum successfully removed by DBE via a water immersion technique.
Case Description/Methods: A 43 year old female s/p sleeve gastrectomy developed a symptomatic gastric body stricture, so a 12 cm fully covered self-expanding metal stent (Hanarostent 22) was placed.
5 weeks later she awoke with severe persistent abdominal pain and presented to the ED for further evaluation.
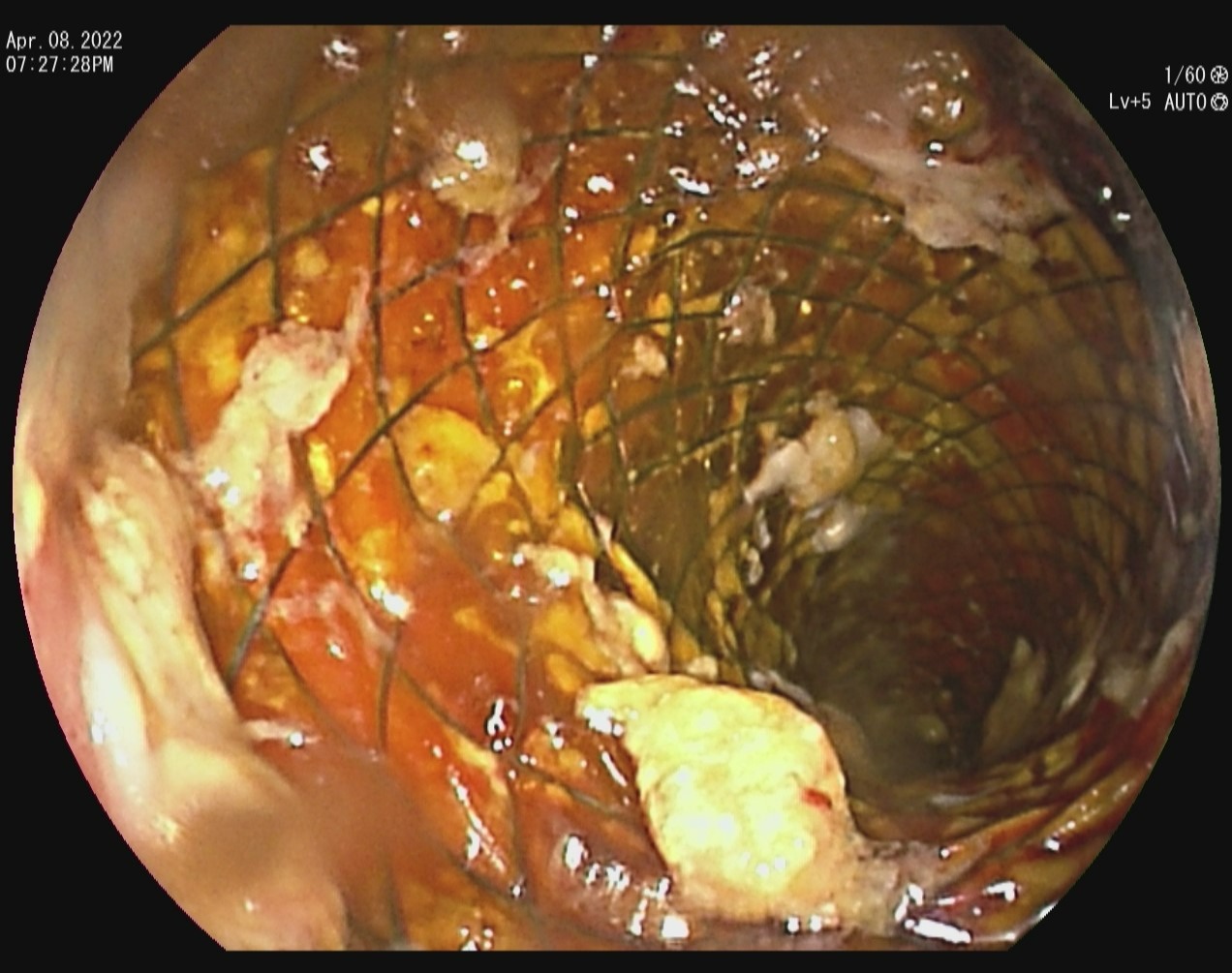
CT abd revealed stent migration to the distal jejunum, with proximal dilation and proximal ascending colon compression by the small bowel loop containing the stent. Anterograde DBE was performed and revealed multiple serpiginous ulcers and large deep ulcers. The stent was embedded into the distal jejunal mucosa, 310 cm distal to the pylorus. Attempts to collapse the stent by pulling the retrieval lasso with a forceps failed after the strings snapped, making stent removal challenging.
A 30 mm Snare was used to collapse the stent head and the proximal portion of the stent. The stent was slowly retracted proximally. However, due to distal stent expansion and small bowel tortuosity, stent retraction was repeatedly retarded at jejunal turns, giving concern for further mucosal trauma.
To maintain bowel distension and decrease trauma, the enteroscope balloon was inflated to 2/3 its normal capacity and water was infused to distend the jejunal lumen. These maneuvers enabled the stent to be safely extracted by keeping the lumen patent, reducing turn angulation, and minimizing trauma to the ulcerated small bowel walls. The stent was successfully extracted and a CT scan revealed no mucosal damage or evidence of perforation. The patient’s pain was immediately alleviated.
Discussion: This case of endoscopic removal of distal jejunal stent migration was complicated severe mucosal ulceration and failure of the stent repositioning device. The water infusion and semi-inflated enteroscope balloon technique enabled safe extraction. To our knowledge, this technique has not previously been described in the literature.
Disclosures:
Otis Stephen, MD. D0461 - Migrated Esophageal Stent Obstructing the Distal Jejunum, Safely Removed by Double-Balloon Enteroscopy Using a Water Immersion Technique, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Cedars Sinai Medical Center, Los Angeles, CA
Introduction: Self-expanding esophageal metal stents are now also used for treatment of gastric and duodenal lesions. Stent migration is a potential risk. Endoscopic retrieval after distal small bowel migration is challenging, often requiring surgery. Double-Balloon Enteroscopy (DBE) enables endoscopic access throughout the small bowel, but small bowel tortuosity makes retrieval of stents in the distal small bowel extremely challenging, so it is performed infrequently.
We describe a case of migration of a fully covered metal stent to the distal jejunum successfully removed by DBE via a water immersion technique.
Case Description/Methods: A 43 year old female s/p sleeve gastrectomy developed a symptomatic gastric body stricture, so a 12 cm fully covered self-expanding metal stent (Hanarostent 22) was placed.
5 weeks later she awoke with severe persistent abdominal pain and presented to the ED for further evaluation.
CT abd revealed stent migration to the distal jejunum, with proximal dilation and proximal ascending colon compression by the small bowel loop containing the stent. Anterograde DBE was performed and revealed multiple serpiginous ulcers and large deep ulcers. The stent was embedded into the distal jejunal mucosa, 310 cm distal to the pylorus. Attempts to collapse the stent by pulling the retrieval lasso with a forceps failed after the strings snapped, making stent removal challenging.
A 30 mm Snare was used to collapse the stent head and the proximal portion of the stent. The stent was slowly retracted proximally. However, due to distal stent expansion and small bowel tortuosity, stent retraction was repeatedly retarded at jejunal turns, giving concern for further mucosal trauma.
To maintain bowel distension and decrease trauma, the enteroscope balloon was inflated to 2/3 its normal capacity and water was infused to distend the jejunal lumen. These maneuvers enabled the stent to be safely extracted by keeping the lumen patent, reducing turn angulation, and minimizing trauma to the ulcerated small bowel walls. The stent was successfully extracted and a CT scan revealed no mucosal damage or evidence of perforation. The patient’s pain was immediately alleviated.
Discussion: This case of endoscopic removal of distal jejunal stent migration was complicated severe mucosal ulceration and failure of the stent repositioning device. The water infusion and semi-inflated enteroscope balloon technique enabled safe extraction. To our knowledge, this technique has not previously been described in the literature.
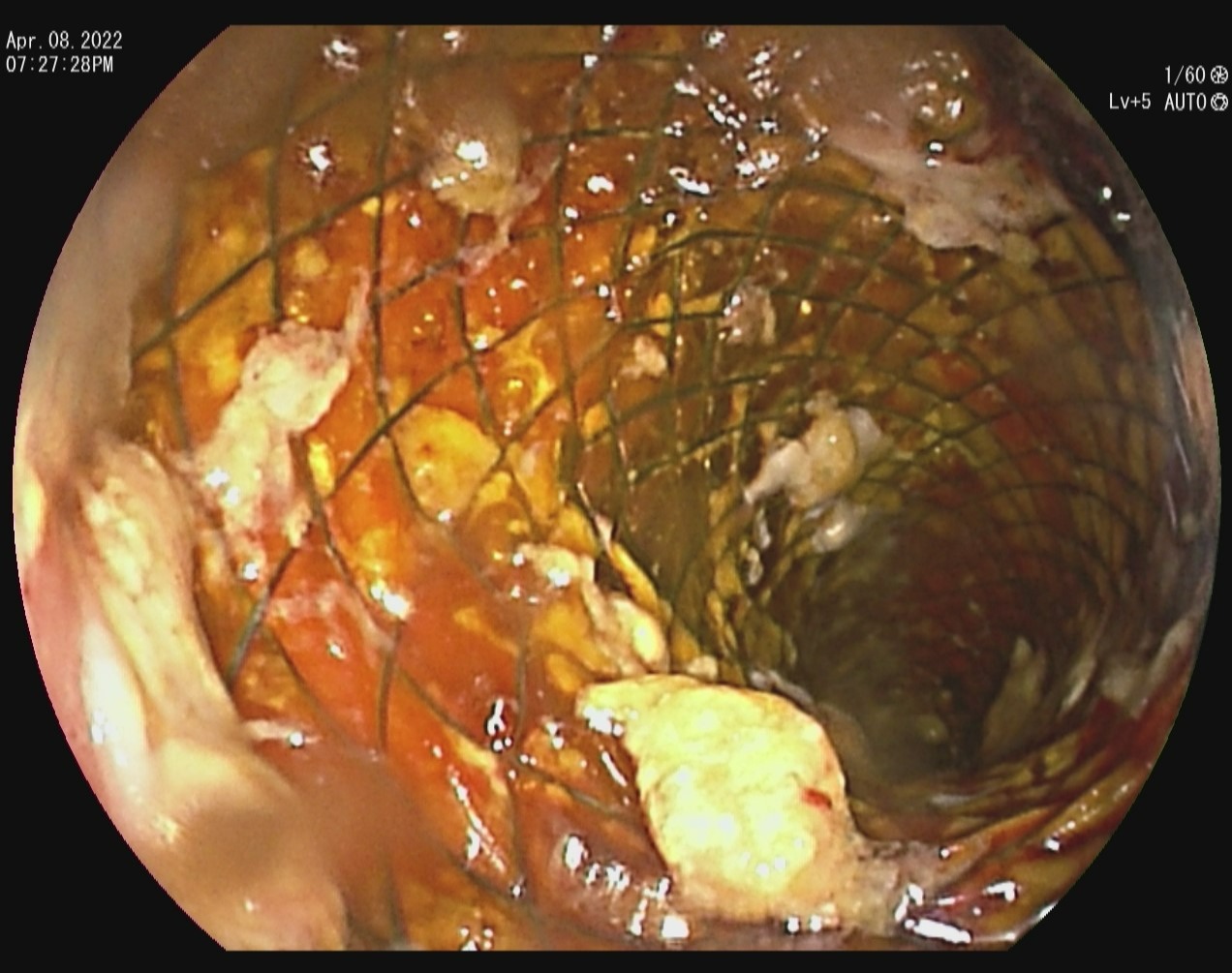
Figure: Stent migrated into the distal jejunum
Disclosures:
Otis Stephen indicated no relevant financial relationships.
Otis Stephen, MD. D0461 - Migrated Esophageal Stent Obstructing the Distal Jejunum, Safely Removed by Double-Balloon Enteroscopy Using a Water Immersion Technique, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
