Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0031 - Not All Gastroparesis Is Gastroparesis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Praneeth Kudaravalli, MD
Augusta University Medical Center
Augusta, GA
Presenting Author(s)
Praneeth Kudaravalli, MD1, Aneesha Gummadi, MS2, Viveksandeep Chandrasekar, MBBS3, John Erikson L. Yap, MD3, Subbaramiah Sridhar, MBBS, MPH4, Satish Rao, MD2
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA; 3Augusta University Medical College of Georiga, Augusta, GA; 4Medical College of Georgia, Augusta, GA
Introduction: Gastroparesis is delayed gastric emptying in the absence of mechanical obstruction. Over 4 million people in the US suffer from the disease with the most common etiology being idiopathic followed by diabetes. Mimickers of gastroparesis need to be ruled to appropriately treat the patient. We present one such case of what was originally thought to be gastroparesis but found to have pancreatic adenocarcinoma causing small bowel obstruction.
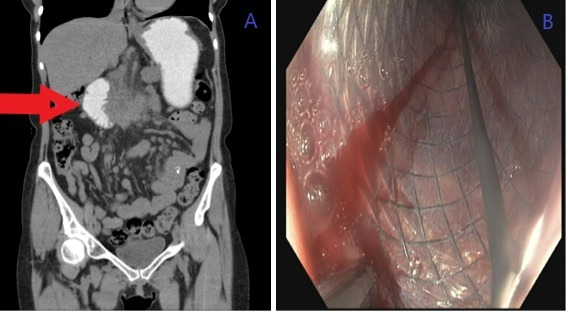
Case Description/Methods: A 62-year-old female with a past medical history of recurrent gallstone pancreatitis status post cholecystectomy presented with symptoms of nausea, vomiting, bloating, reflux, and 22lb weight loss. A gastric emptying study done at a local hospital showed 95% retention after 4 hours. She underwent a feeding jejunostomy with venting. Because of presumed persistent gastroparesis, and repeated hospitalization she was scheduled for gastric pacemaker placement at outside facility. Patient sought a second opinion in our motility clinic. Physical exam was significant for a succussion splash. A CT abdomen showed an ill-defined soft tissue structure centered at the pancreaticoduodenal groove with associated duodenal stenosis (Image A) – indicating groove pancreatitis. EGD showed complete obstruction of the 2nd portion of the duodenum. Initial stricture biopsies were benign. Following this, balloon dilation was performed and a 20 mm X 12cm fully covered metal stent (Image B) was placed. Patient however continued to report symptoms of nausea and vomiting with new onset of jaundice. Repeat CT abdomen demonstrated distal CBD obstruction with upstream dilation. Patient underwent PTC drain placement, and CBD brush biopsy obtained demonstrated non-viable cells without evidence of malignancy. Labs revealed normal lipase and IgG4 levels. Given non-resolution of pancreatic inflammation, to rule out malignancy, it was decided to perform EUS with FNA which showed pancreatic head adenocarcinoma with duodenal infiltration.
Discussion: Groove pancreatitis affects the anatomical area between the head of the pancreas, duodenum, and common bile duct. Common complications include biliary stricture with obstructive jaundice and duodenal stricture. In our case, the duodenal stricture caused secondary gastroparesis. Groove pancreatitis and pancreatic adenocarcinoma are challenging to differentiate with similar presentation. It is important to differentiate a benign from a malignant etiology as treatment and prognosis varies significantly.
Disclosures:
Praneeth Kudaravalli, MD1, Aneesha Gummadi, MS2, Viveksandeep Chandrasekar, MBBS3, John Erikson L. Yap, MD3, Subbaramiah Sridhar, MBBS, MPH4, Satish Rao, MD2. A0031 - Not All Gastroparesis Is Gastroparesis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Augusta University Medical Center, Augusta, GA; 2Augusta University, Augusta, GA; 3Augusta University Medical College of Georiga, Augusta, GA; 4Medical College of Georgia, Augusta, GA
Introduction: Gastroparesis is delayed gastric emptying in the absence of mechanical obstruction. Over 4 million people in the US suffer from the disease with the most common etiology being idiopathic followed by diabetes. Mimickers of gastroparesis need to be ruled to appropriately treat the patient. We present one such case of what was originally thought to be gastroparesis but found to have pancreatic adenocarcinoma causing small bowel obstruction.
Case Description/Methods: A 62-year-old female with a past medical history of recurrent gallstone pancreatitis status post cholecystectomy presented with symptoms of nausea, vomiting, bloating, reflux, and 22lb weight loss. A gastric emptying study done at a local hospital showed 95% retention after 4 hours. She underwent a feeding jejunostomy with venting. Because of presumed persistent gastroparesis, and repeated hospitalization she was scheduled for gastric pacemaker placement at outside facility. Patient sought a second opinion in our motility clinic. Physical exam was significant for a succussion splash. A CT abdomen showed an ill-defined soft tissue structure centered at the pancreaticoduodenal groove with associated duodenal stenosis (Image A) – indicating groove pancreatitis. EGD showed complete obstruction of the 2nd portion of the duodenum. Initial stricture biopsies were benign. Following this, balloon dilation was performed and a 20 mm X 12cm fully covered metal stent (Image B) was placed. Patient however continued to report symptoms of nausea and vomiting with new onset of jaundice. Repeat CT abdomen demonstrated distal CBD obstruction with upstream dilation. Patient underwent PTC drain placement, and CBD brush biopsy obtained demonstrated non-viable cells without evidence of malignancy. Labs revealed normal lipase and IgG4 levels. Given non-resolution of pancreatic inflammation, to rule out malignancy, it was decided to perform EUS with FNA which showed pancreatic head adenocarcinoma with duodenal infiltration.
Discussion: Groove pancreatitis affects the anatomical area between the head of the pancreas, duodenum, and common bile duct. Common complications include biliary stricture with obstructive jaundice and duodenal stricture. In our case, the duodenal stricture caused secondary gastroparesis. Groove pancreatitis and pancreatic adenocarcinoma are challenging to differentiate with similar presentation. It is important to differentiate a benign from a malignant etiology as treatment and prognosis varies significantly.
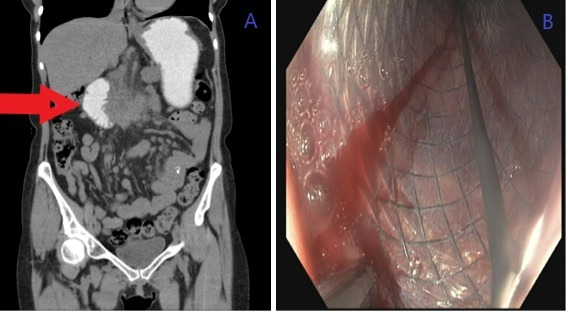
Figure: Image 1 (A) – Red arrow shows the area of abrupt duodenal narrowing with proximal duodenum and stomach showing opacification with oral contrast. (B) - 20 mm wide X 12 cm long fully covered metal stent at the site of duodenal stricture.
Disclosures:
Praneeth Kudaravalli indicated no relevant financial relationships.
Aneesha Gummadi indicated no relevant financial relationships.
Viveksandeep Chandrasekar indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Subbaramiah Sridhar indicated no relevant financial relationships.
Satish Rao: Salix Pharmaceuticals – Grant/Research Support. Vibrant – Advisor or Review Panel Member. Vibrant – Clinical Advisory Board.
Praneeth Kudaravalli, MD1, Aneesha Gummadi, MS2, Viveksandeep Chandrasekar, MBBS3, John Erikson L. Yap, MD3, Subbaramiah Sridhar, MBBS, MPH4, Satish Rao, MD2. A0031 - Not All Gastroparesis Is Gastroparesis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
