Back

Poster Session E - Tuesday Afternoon
Category: Colon
E0147 - A Uncommon Presentation of Invasive Colonic Amebiasis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sherlon Orin O. Sinclair, MD
Harlem Hospital Center
New York, NY
Presenting Author(s)
Sherlon Orin O. Sinclair, MD, Joan A. Culpepper-Morgan, MD, FACG
Harlem Hospital Center, New York, NY
Introduction: Intestinal parasitic infections are more common in developing countries. There is an increased risk for morbidity and mortality in individuals with certain risk factors, such as HIV, due to related enteropathy, favoring parasitic intestinal colonization. When symptomatic, most cases of amebic colitis present with abdominal pain, diarrhoea and/or hematochezia. We present a case of an asymptomatic female immigrant with HIV, who was found to have invasive cecal amebiasis on screening colonoscopy.
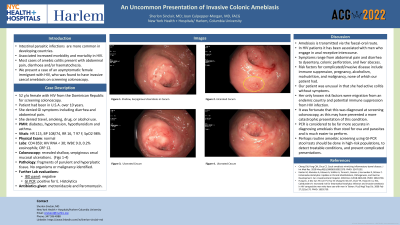
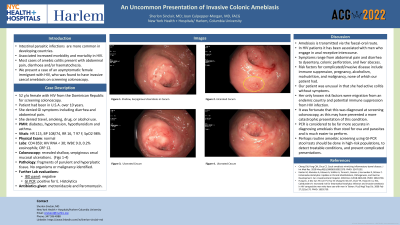
Case Description/Methods: A 52 y/o lady presented to GI clinic for screening colonoscopy. She has a PMH of HIV, diabetes, hypertension, hypothyroidism and asthma. She was asymptomatic and denied GI symptoms, travel, smoking or illicit drug/alcohol use. She migrated from Dominican Republic many years ago, and denied any episodes of diarrhoea or abdominal pain. Her vitals were HR 115, BP 108/74, RR 16, T 97 F, SpO2 98%, and she had a normal physical exam. Labs: CD4 859, HIV RNA < 30; WBC 9, 0.2% eosin, CRP 12. She proceeded to have colonoscopy which revealed a hyperplastic polyp and shallow, serpiginous cecal mucosal ulcerations, negative for malignancy. At follow up, she again denied GI symptoms and had a benign abdominal exam. An IBD panel and GI PCR panel were tested to assess for possible infective/inflammatory causes. GI panel was positive for E. Histolytica, and coupled with the characteristic cecal ulcerations, a diagnosis of invasive intestinal amebiasis was made, for which she was treated with antibiotics.
Discussion: Amebic colitis in HIV patients usually affects men who have sex with men due to fecal-oral transmission from anal/oral sex. It often presents with abdominal pain, diarrhoea, or in severe cases, peritonitis from colonic perforation. Some risk factors for complicated/invasive infections are alcoholism, malnutrition, and malignancy. What makes our case unique is the presence of invasive amebic colitis in an asymptomatic female patient with HIV, and no history of anal sex, malignancy, or alcoholism. Her only risk factors were migration from a developing country and HIV infection, albeit well controlled, reflected by favourable CD4 count and viral load. It was fortunate that she was eligible for screening colonoscopy as it yielded findings of an invasive infective colitis, requiring treatment, and possibly prevented a more catastrophic presentation as a consequence of colonic perforation. This brings into question the possible role for routine amebic screening in high-risk populations.

Disclosures:
Sherlon Orin O. Sinclair, MD, Joan A. Culpepper-Morgan, MD, FACG. E0147 - A Uncommon Presentation of Invasive Colonic Amebiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Harlem Hospital Center, New York, NY
Introduction: Intestinal parasitic infections are more common in developing countries. There is an increased risk for morbidity and mortality in individuals with certain risk factors, such as HIV, due to related enteropathy, favoring parasitic intestinal colonization. When symptomatic, most cases of amebic colitis present with abdominal pain, diarrhoea and/or hematochezia. We present a case of an asymptomatic female immigrant with HIV, who was found to have invasive cecal amebiasis on screening colonoscopy.
Case Description/Methods: A 52 y/o lady presented to GI clinic for screening colonoscopy. She has a PMH of HIV, diabetes, hypertension, hypothyroidism and asthma. She was asymptomatic and denied GI symptoms, travel, smoking or illicit drug/alcohol use. She migrated from Dominican Republic many years ago, and denied any episodes of diarrhoea or abdominal pain. Her vitals were HR 115, BP 108/74, RR 16, T 97 F, SpO2 98%, and she had a normal physical exam. Labs: CD4 859, HIV RNA < 30; WBC 9, 0.2% eosin, CRP 12. She proceeded to have colonoscopy which revealed a hyperplastic polyp and shallow, serpiginous cecal mucosal ulcerations, negative for malignancy. At follow up, she again denied GI symptoms and had a benign abdominal exam. An IBD panel and GI PCR panel were tested to assess for possible infective/inflammatory causes. GI panel was positive for E. Histolytica, and coupled with the characteristic cecal ulcerations, a diagnosis of invasive intestinal amebiasis was made, for which she was treated with antibiotics.
Discussion: Amebic colitis in HIV patients usually affects men who have sex with men due to fecal-oral transmission from anal/oral sex. It often presents with abdominal pain, diarrhoea, or in severe cases, peritonitis from colonic perforation. Some risk factors for complicated/invasive infections are alcoholism, malnutrition, and malignancy. What makes our case unique is the presence of invasive amebic colitis in an asymptomatic female patient with HIV, and no history of anal sex, malignancy, or alcoholism. Her only risk factors were migration from a developing country and HIV infection, albeit well controlled, reflected by favourable CD4 count and viral load. It was fortunate that she was eligible for screening colonoscopy as it yielded findings of an invasive infective colitis, requiring treatment, and possibly prevented a more catastrophic presentation as a consequence of colonic perforation. This brings into question the possible role for routine amebic screening in high-risk populations.

Figure: Continuous area of shallow, serpiginous ulcerated mucosa in the cecum, with stigmata of recent bleeding.
Disclosures:
Sherlon Orin Sinclair indicated no relevant financial relationships.
Joan Culpepper-Morgan indicated no relevant financial relationships.
Sherlon Orin O. Sinclair, MD, Joan A. Culpepper-Morgan, MD, FACG. E0147 - A Uncommon Presentation of Invasive Colonic Amebiasis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

