Back

Poster Session D - Tuesday Morning
Category: General Endoscopy
D0298 - Hit Me With Your Best Shot: Splenic Laceration Post Colonoscopy
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Idrees Suliman, MD
Mountain Vista Medical Center
Mesa, AZ
Presenting Author(s)
Preeyanka Sundar, MD1, Suma Harsha Kosuru, MBBS1, Idrees Suliman, MD2, Sara Ancello, DO1
1Midwestern University, Mesa, AZ; 2Mountain Vista Medical Center, Mesa, AZ
Introduction: With more than 16 million colonoscopies conducted each year in the United States, colonoscopy is the gold standard for detecting any colonic pathology. The most common complications described are intraluminal hemorrhage (0.3–2.1%) and colonic (micro)perforation (0.1–2.5%). Splenic injury during colonoscopy was initially identified by Wherry and Zehner as a rare but life-threatening event. Here, we discuss a case of post colonoscopy splenic laceration associated with multiple polypectomies.
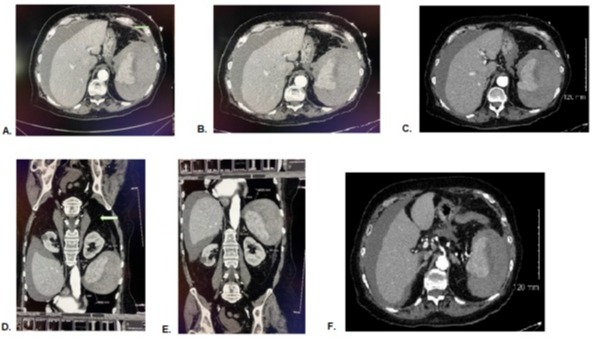
Case Description/Methods: 74-year-old female with hypertension, hyperlipidemia, on no blood thinners, presented 3 days after screening colonoscopy (16 polyps removed) to the hospital with complaints of left upper quadrant abdominal pain, weakness and fatigue without any GI bleeding. Of note, a previous colonoscopy 3 years ago with 18 removed, all benign, was uneventful. All her polyps were sub centimeter, required only hot and cold snare, no endoscopic mucosal resection. Labs demonstrated hemoglobin of 7gm/dl, WBC 15.5K, creatinine 1.7, lactic acid 2.2, and CT the abdomen revealed 3 cm splenic laceration grade 3 with subcapsular hematoma without bleeding (Figure 1). She was transfused 2 units of packed cells with improvement of her hemoglobin to 10.0 after which her blood count remained stable, she was monitored and treated for pain, and discharged successfully home after 2 days with instruction to avoid high-impact activities which could result in further trauma to the spleen.
Discussion: Splenic injury has an incidence ranging from 1 in 100,000 to 1 in 6,387 colonoscopies . The mortality rate for a traumatic splenic injury requiring splenectomy has been reported to be 25%. Advanced age, with an average age of 63.0 years, is thought to be a risk factor for splenic damage, with female patients accounting for 72–75 percent of splenic injuries after colonoscopy. The most likely causes being excessive manipulation done to advance the scope beyond the splenic flexure or traction on the splenocolic ligament. A higher incidence has been observed when biopsies or polypectomies were performed during therapeutic colonoscopies, with polypectomy accounting for a 7-fold increase risk of adverse events. This complication may be avoided with a left lateral position and minimizing the external pressure. Henceforth, we would like to draw your attention to the fact that a clinician should be extra cautious while doing these maneuvers since, while it is a rare complication, it can be life threatening.
Disclosures:
Preeyanka Sundar, MD1, Suma Harsha Kosuru, MBBS1, Idrees Suliman, MD2, Sara Ancello, DO1. D0298 - Hit Me With Your Best Shot: Splenic Laceration Post Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Midwestern University, Mesa, AZ; 2Mountain Vista Medical Center, Mesa, AZ
Introduction: With more than 16 million colonoscopies conducted each year in the United States, colonoscopy is the gold standard for detecting any colonic pathology. The most common complications described are intraluminal hemorrhage (0.3–2.1%) and colonic (micro)perforation (0.1–2.5%). Splenic injury during colonoscopy was initially identified by Wherry and Zehner as a rare but life-threatening event. Here, we discuss a case of post colonoscopy splenic laceration associated with multiple polypectomies.
Case Description/Methods: 74-year-old female with hypertension, hyperlipidemia, on no blood thinners, presented 3 days after screening colonoscopy (16 polyps removed) to the hospital with complaints of left upper quadrant abdominal pain, weakness and fatigue without any GI bleeding. Of note, a previous colonoscopy 3 years ago with 18 removed, all benign, was uneventful. All her polyps were sub centimeter, required only hot and cold snare, no endoscopic mucosal resection. Labs demonstrated hemoglobin of 7gm/dl, WBC 15.5K, creatinine 1.7, lactic acid 2.2, and CT the abdomen revealed 3 cm splenic laceration grade 3 with subcapsular hematoma without bleeding (Figure 1). She was transfused 2 units of packed cells with improvement of her hemoglobin to 10.0 after which her blood count remained stable, she was monitored and treated for pain, and discharged successfully home after 2 days with instruction to avoid high-impact activities which could result in further trauma to the spleen.
Discussion: Splenic injury has an incidence ranging from 1 in 100,000 to 1 in 6,387 colonoscopies . The mortality rate for a traumatic splenic injury requiring splenectomy has been reported to be 25%. Advanced age, with an average age of 63.0 years, is thought to be a risk factor for splenic damage, with female patients accounting for 72–75 percent of splenic injuries after colonoscopy. The most likely causes being excessive manipulation done to advance the scope beyond the splenic flexure or traction on the splenocolic ligament. A higher incidence has been observed when biopsies or polypectomies were performed during therapeutic colonoscopies, with polypectomy accounting for a 7-fold increase risk of adverse events. This complication may be avoided with a left lateral position and minimizing the external pressure. Henceforth, we would like to draw your attention to the fact that a clinician should be extra cautious while doing these maneuvers since, while it is a rare complication, it can be life threatening.
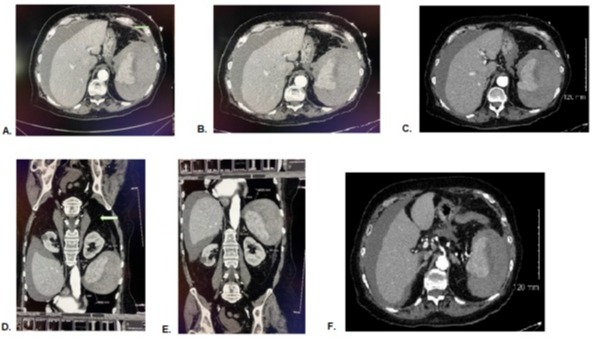
Figure: Figure1: A-F - Coronal view of linear lucencies within the spleen suggestive of lacerations. The largest measures 3 cm. There is also an 11 cm subcapsular splenic hematoma. There is no evidence of acute contrast blush. Findings are consistent with grade 3 splenic injury.
Disclosures:
Preeyanka Sundar indicated no relevant financial relationships.
Suma Harsha Kosuru indicated no relevant financial relationships.
Idrees Suliman indicated no relevant financial relationships.
Sara Ancello indicated no relevant financial relationships.
Preeyanka Sundar, MD1, Suma Harsha Kosuru, MBBS1, Idrees Suliman, MD2, Sara Ancello, DO1. D0298 - Hit Me With Your Best Shot: Splenic Laceration Post Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
