Back

Poster Session E - Tuesday Afternoon
Category: Esophagus
E0231 - The Odd Couple: Active H. pylori Infection Within Long Segment Barrett’s Esophagus
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Rei Mitsuyama, MD
Brown University
Providence, RI
Presenting Author(s)
Rei Mitsuyama, MD1, Weibiao Cao, MD1, Sarah M. Hyder, MD, MBA2
1Brown University, Providence, RI; 2Lifespan Physician Group - Brown University, East Providence, RI
Introduction: Barrett’s esophagus (BE) is a consequence of poorly-controlled GERD leading to intestinal metaplasia, which predisposes to esophageal cancer. Similarly, there is a well-established link between Helicobacter pylori and development of gastric cancer. However, there is a negative association between H pylori and risk of BE. Here, we present a rare case of H Pylori infection within Barrett's mucosa.
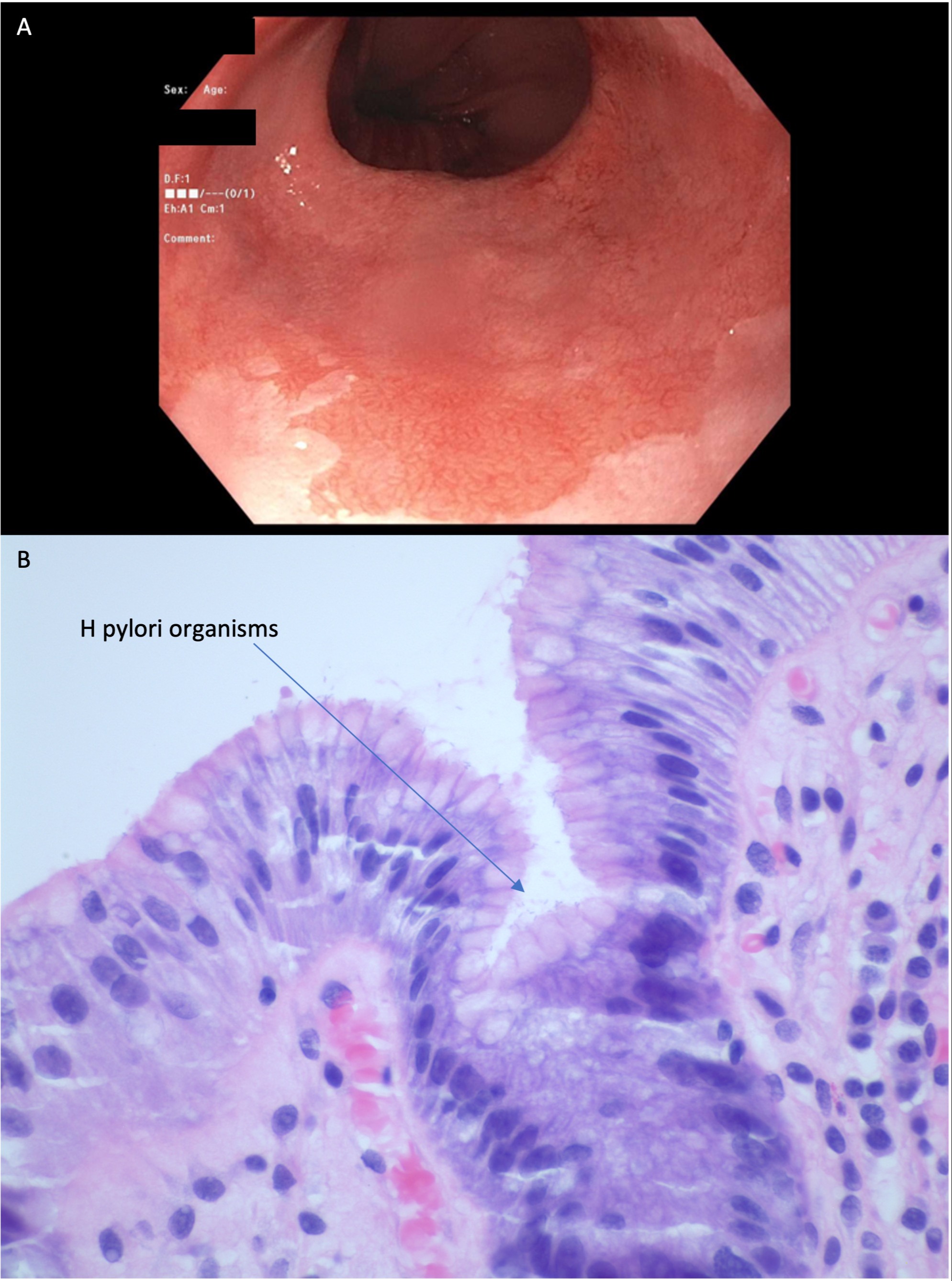
Case Description/Methods: A 54-year-old woman was referred for one month of dysphagia to solids. She described food sticking in her mid-esophagus without difficulty swallowing pills or liquids. She also endorsed significant heartburn and belching but denied systemic symptoms, regurgitation, abdominal pain, or weight loss. EGD demonstrated a 5 cm segment of circumferential salmon-colored mucosa suspicious for Barrett’s esophagus, a small esophageal ulcer, and a normal stomach and duodenum. Gastric biopsies revealed mild gastritis with H pylori organisms. Esophageal biopsies showed intestinal metaplasia consistent with Barrett’s esophagus as well as H pylori organisms. Quadruple therapy was initiated with metronidazole, tetracycline, omeprazole, and bismuth.
Discussion: We describe a rare case of H pylori discovered within long-segment Barrett’s esophagus. Evidence suggests an inverse association between H pylori and BE. However, a recent meta-analysis demonstrated that this association disappeared in patients with GERD. One proposed mechanism for H pylori’s protectiveness against BE is decreased gastric acid production. Together, this suggests H pylori protects against BE by preventing development of GERD but once GERD is present, H pylori is no longer protective. Thus, our simultaneous diagnosis of BE and H pylori could be explained by long-standing GERD and BE prior to H pylori infection.
While it is uncommon to diagnose H pylori and BE together, it is even rarer to see H pylori within Barrett’s mucosa, given the organism’s proclivity for gastric epithelium. One potential explanation is that this patient’s significant GERD allowed reflux of H pylori organisms into the esophagus, leading to colonization of the metaplastic epithelium. Furthermore, there may be microscopic satellites of gastric mucosa within the segment of BE, providing a friendlier environment in which the organisms could grow.
More observation is needed to determine the significance and long term effects of active H pylori infection in Barrett's mucosa and if this facilitates progression to dysplasia or carcinoma.
Disclosures:
Rei Mitsuyama, MD1, Weibiao Cao, MD1, Sarah M. Hyder, MD, MBA2. E0231 - The Odd Couple: Active H. pylori Infection Within Long Segment Barrett’s Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Brown University, Providence, RI; 2Lifespan Physician Group - Brown University, East Providence, RI
Introduction: Barrett’s esophagus (BE) is a consequence of poorly-controlled GERD leading to intestinal metaplasia, which predisposes to esophageal cancer. Similarly, there is a well-established link between Helicobacter pylori and development of gastric cancer. However, there is a negative association between H pylori and risk of BE. Here, we present a rare case of H Pylori infection within Barrett's mucosa.
Case Description/Methods: A 54-year-old woman was referred for one month of dysphagia to solids. She described food sticking in her mid-esophagus without difficulty swallowing pills or liquids. She also endorsed significant heartburn and belching but denied systemic symptoms, regurgitation, abdominal pain, or weight loss. EGD demonstrated a 5 cm segment of circumferential salmon-colored mucosa suspicious for Barrett’s esophagus, a small esophageal ulcer, and a normal stomach and duodenum. Gastric biopsies revealed mild gastritis with H pylori organisms. Esophageal biopsies showed intestinal metaplasia consistent with Barrett’s esophagus as well as H pylori organisms. Quadruple therapy was initiated with metronidazole, tetracycline, omeprazole, and bismuth.
Discussion: We describe a rare case of H pylori discovered within long-segment Barrett’s esophagus. Evidence suggests an inverse association between H pylori and BE. However, a recent meta-analysis demonstrated that this association disappeared in patients with GERD. One proposed mechanism for H pylori’s protectiveness against BE is decreased gastric acid production. Together, this suggests H pylori protects against BE by preventing development of GERD but once GERD is present, H pylori is no longer protective. Thus, our simultaneous diagnosis of BE and H pylori could be explained by long-standing GERD and BE prior to H pylori infection.
While it is uncommon to diagnose H pylori and BE together, it is even rarer to see H pylori within Barrett’s mucosa, given the organism’s proclivity for gastric epithelium. One potential explanation is that this patient’s significant GERD allowed reflux of H pylori organisms into the esophagus, leading to colonization of the metaplastic epithelium. Furthermore, there may be microscopic satellites of gastric mucosa within the segment of BE, providing a friendlier environment in which the organisms could grow.
More observation is needed to determine the significance and long term effects of active H pylori infection in Barrett's mucosa and if this facilitates progression to dysplasia or carcinoma.
Figure: Figure 1. A. Esophagoduodenoscopy (EGD) image of 5 cm circumferential salmon mucosa consistent with Barrett’s esophagus. B. Hematoxylin and eosin (H&E) stain of esophageal mucosa demonstrating intestinal metaplasia and H pylori organisms.
Disclosures:
Rei Mitsuyama indicated no relevant financial relationships.
Weibiao Cao indicated no relevant financial relationships.
Sarah Hyder indicated no relevant financial relationships.
Rei Mitsuyama, MD1, Weibiao Cao, MD1, Sarah M. Hyder, MD, MBA2. E0231 - The Odd Couple: Active H. pylori Infection Within Long Segment Barrett’s Esophagus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
