Back

Poster Session E - Tuesday Afternoon
Category: Functional Bowel Disease
E0258 - Loss of Bifidobacteria in Lyme Disease: Cause or Effect
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sabine Hazan, MD
ProgenaBiome, LLC
VENTURA, CA
Presenting Author(s)
Sabine Hazan, MD1, Sonya Dave, PhD2, Amelia Goudzwaard, 3, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG4
1ProgenaBiome, LLC, Ventura, CA; 2North End Advisory, Smyrna, GA; 3University of Southern California, Los Angeles, CA; 4Centre for Digestive Diseases, Five Dock, New South Wales, Australia
Introduction: Lyme disease is a poorly understood condition which starts with a rash but may continue with chronic fatigue and neurological symptoms. Approximately 1 in 5 early Lyme disease patients have GI symptoms, such as nausea, anorexia, abdominal pain, or diarrhea. Lyme disease is thought to be cased by microbes in the spirochetes phylum transmitted by black legged ticks. Lyme-related healthcare costs in America exceed 1.3 billion dollars annually.
Bifidobacteria are known for their beneficial probiotic actions within the human gut microbiome. Their numbers are reduced in severe COVID-19, Clostridioides difficile infection and Inflammatory Bowel Disease.
To our knowledge Bifidobacteria levels have not been studied in Lyme disease patients. Given the importance of Bifidobacterium abundance in other diseases, we focused on relative abundance of Bifidobacterium in fecal samples of patients with Lyme disease compared to controls.
Methods: Fecal samples were assessed for relative abundance of Bifidobacterium in Healthy Control subjects without Lyme disease (n=20) compared to patients with Lyme disease (n=39). The average symptom duration in patients with Lyme disease was 5 years and none were on antibiotics 2 weeks prior to sample collection (range of symptoms from 1 month to 20 years, all treated initially with antibiotics).
Metagenomics Next Generation sequencing was performed on fecal samples, where DNA samples were extracted and normalized for library downstream analysis using Shotgun Methodology. Mann-Whitney Statistical test was used for comparison.
This study was IRB approved.
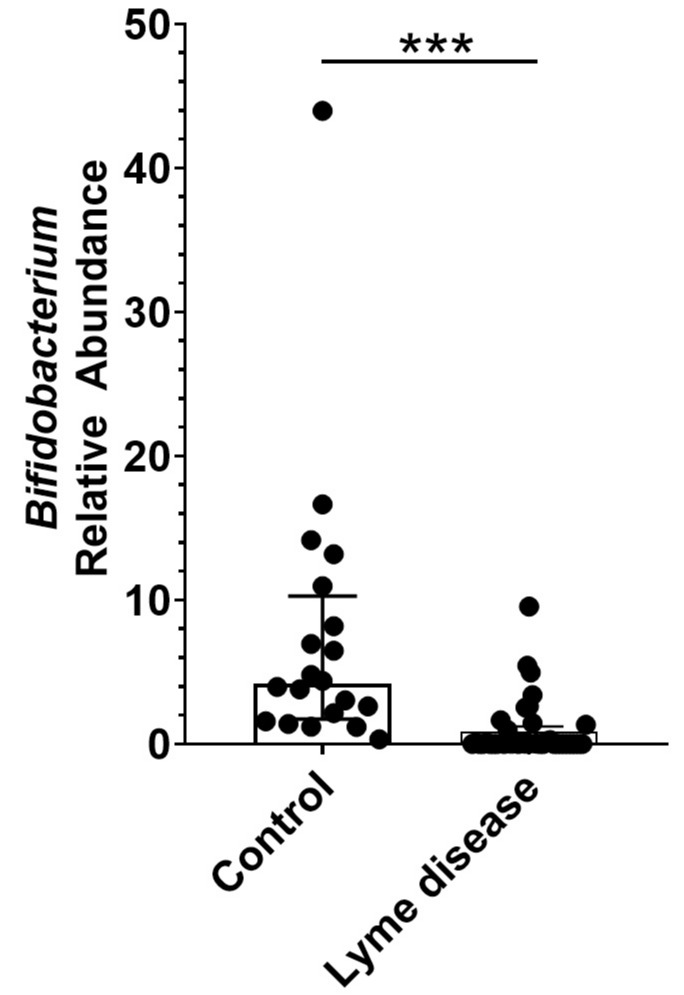
Results: Relative Abundance of bifidobacteria was significantly decreased (p< 0.0001) in patients with Lyme disease. Median and interquartile range (IQR) were: Control (Median:4.175%; IQR:1.72-10.27%) and Lyme disease (Median:0.0014%; IQR:0.00%-0.96%)(Figure 1). 30/39 Lyme disease patients (77%) were found to possess < 1% relative abundance of Bifidobacterium in their stool sample. Of interest only 1/39 samples showed presence of Spirochetes in stool samples.
Discussion: This is the first study that demonstrates low levels of Bifidobacteria in patients with chronic Lyme disease. These results raise three questions; whether the disease was caused by 1. the original microbe creating loss of Bifidobacterium 2. baseline low Bifidobacteria due likely to either diet or medications or 3. excessive treatment. Given Lyme disease comprises a gut dysbiosis issue, therapies should also aim at restoration of depleted Bifidobacteria.
Disclosures:
Sabine Hazan, MD1, Sonya Dave, PhD2, Amelia Goudzwaard, 3, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG4. E0258 - Loss of Bifidobacteria in Lyme Disease: Cause or Effect, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1ProgenaBiome, LLC, Ventura, CA; 2North End Advisory, Smyrna, GA; 3University of Southern California, Los Angeles, CA; 4Centre for Digestive Diseases, Five Dock, New South Wales, Australia
Introduction: Lyme disease is a poorly understood condition which starts with a rash but may continue with chronic fatigue and neurological symptoms. Approximately 1 in 5 early Lyme disease patients have GI symptoms, such as nausea, anorexia, abdominal pain, or diarrhea. Lyme disease is thought to be cased by microbes in the spirochetes phylum transmitted by black legged ticks. Lyme-related healthcare costs in America exceed 1.3 billion dollars annually.
Bifidobacteria are known for their beneficial probiotic actions within the human gut microbiome. Their numbers are reduced in severe COVID-19, Clostridioides difficile infection and Inflammatory Bowel Disease.
To our knowledge Bifidobacteria levels have not been studied in Lyme disease patients. Given the importance of Bifidobacterium abundance in other diseases, we focused on relative abundance of Bifidobacterium in fecal samples of patients with Lyme disease compared to controls.
Methods: Fecal samples were assessed for relative abundance of Bifidobacterium in Healthy Control subjects without Lyme disease (n=20) compared to patients with Lyme disease (n=39). The average symptom duration in patients with Lyme disease was 5 years and none were on antibiotics 2 weeks prior to sample collection (range of symptoms from 1 month to 20 years, all treated initially with antibiotics).
Metagenomics Next Generation sequencing was performed on fecal samples, where DNA samples were extracted and normalized for library downstream analysis using Shotgun Methodology. Mann-Whitney Statistical test was used for comparison.
This study was IRB approved.
Results: Relative Abundance of bifidobacteria was significantly decreased (p< 0.0001) in patients with Lyme disease. Median and interquartile range (IQR) were: Control (Median:4.175%; IQR:1.72-10.27%) and Lyme disease (Median:0.0014%; IQR:0.00%-0.96%)(Figure 1). 30/39 Lyme disease patients (77%) were found to possess < 1% relative abundance of Bifidobacterium in their stool sample. Of interest only 1/39 samples showed presence of Spirochetes in stool samples.
Discussion: This is the first study that demonstrates low levels of Bifidobacteria in patients with chronic Lyme disease. These results raise three questions; whether the disease was caused by 1. the original microbe creating loss of Bifidobacterium 2. baseline low Bifidobacteria due likely to either diet or medications or 3. excessive treatment. Given Lyme disease comprises a gut dysbiosis issue, therapies should also aim at restoration of depleted Bifidobacteria.
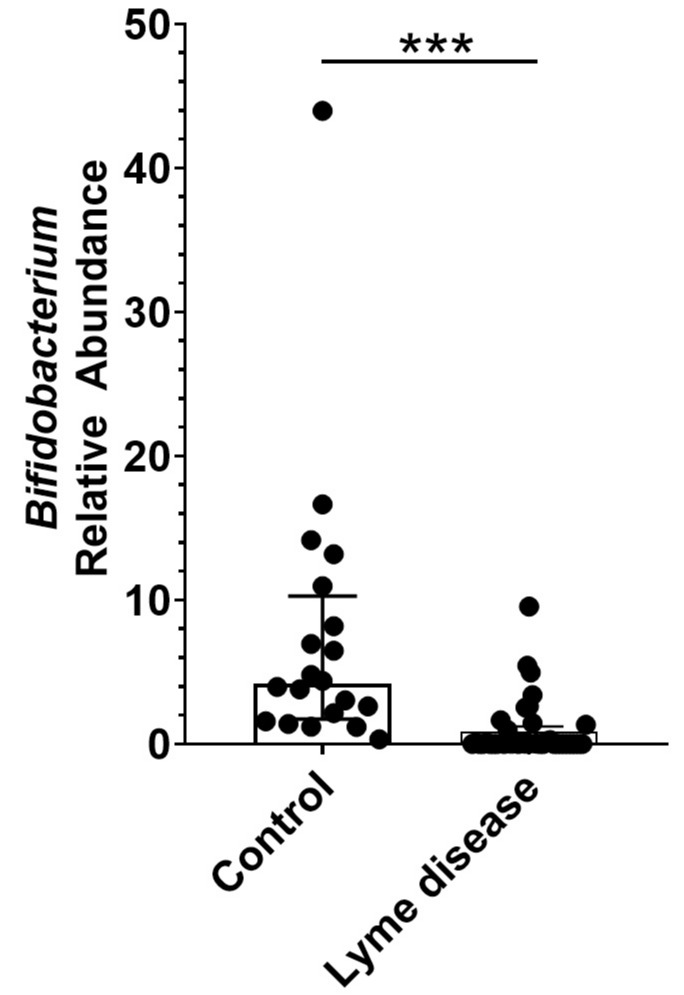
Figure: Figure 1. Lyme disease subjects have significantly (p<0.001) reduced relative abundance of genus bifidobacterium.
Disclosures:
Sabine Hazan indicated no relevant financial relationships.
Sonya Dave: McKesson Specialty Health / Ontada – Employee.
Amelia Goudzwaard indicated no relevant financial relationships.
Brad Barrows indicated no relevant financial relationships.
Thomas Borody: Axent medical Pty. Ltd – Advisory Committee/Board Member. Centre for Digestive Diseases – Advisory Committee/Board Member, Consultant, Employee, Grant/Research Support, Intellectual Property/Patents, Ownership interest, Owner/Ownership Interest, Stock-privately held company. Finch Therapeutics – Advisory Committee/Board Member, Intellectual Property/Patents, Stock-publicly held company(excluding mutual/index funds). Topelia Therapeutics – Advisor or Review Panel Member, Intellectual Property/Patents.
Sabine Hazan, MD1, Sonya Dave, PhD2, Amelia Goudzwaard, 3, Brad Barrows, DO1, Thomas J. Borody, MD, PhD, DSc, FACG4. E0258 - Loss of Bifidobacteria in Lyme Disease: Cause or Effect, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
