Back

Poster Session D - Tuesday Morning
Category: Small Intestine
D0657 - Choledocystoduodenal Fistula Effectively Treated With a High-Dose Proton Pump Inhibitor: A Case Report
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Miguel Lacayo, MD
New York Presbyterian Brooklyn Methodist Hospital
Brooklyn, NY
Presenting Author(s)
Miguel Lacayo, MD, Ezana Bekele, MD, Pratima Dibba, MD, Amar Manvar, MD, Irwin Grosman, MD
New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Choledocystoduodenal fistulas are a rare complication of biliary or peptic ulcer disease. Approximately 91%-94% of spontaneous internal biliary fistulas are caused by stones in the biliary tract. The second most common cause is peptic ulcer. We present a case of a patient found to have a choledocystoduodenal fistula caused by peptic ulcer disease successfully treated with high-dose PPI.
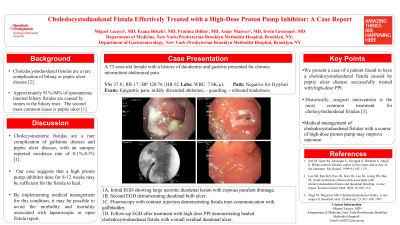
Case Description/Methods: A 73-year-old female with a history of duodenitis and gastritis presented for chronic intermittent abdominal pain. Physical exam was positive for epigastric tenderness. Labs were normal. Imaging revealed a large stool burden, mildly distended gallbladder without gallstones and a normal biliary tree. She was started on a once-daily PPI and a bowel regimen. EGD was performed and demonstrated a large necrotic duodenal lesion with copious purulent drainage (Figure 1A). Gastric biopsy was negative for H. pylori.
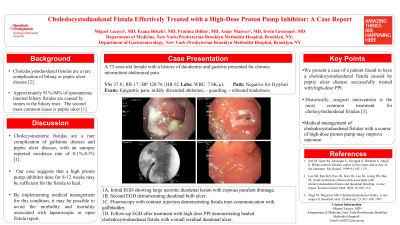
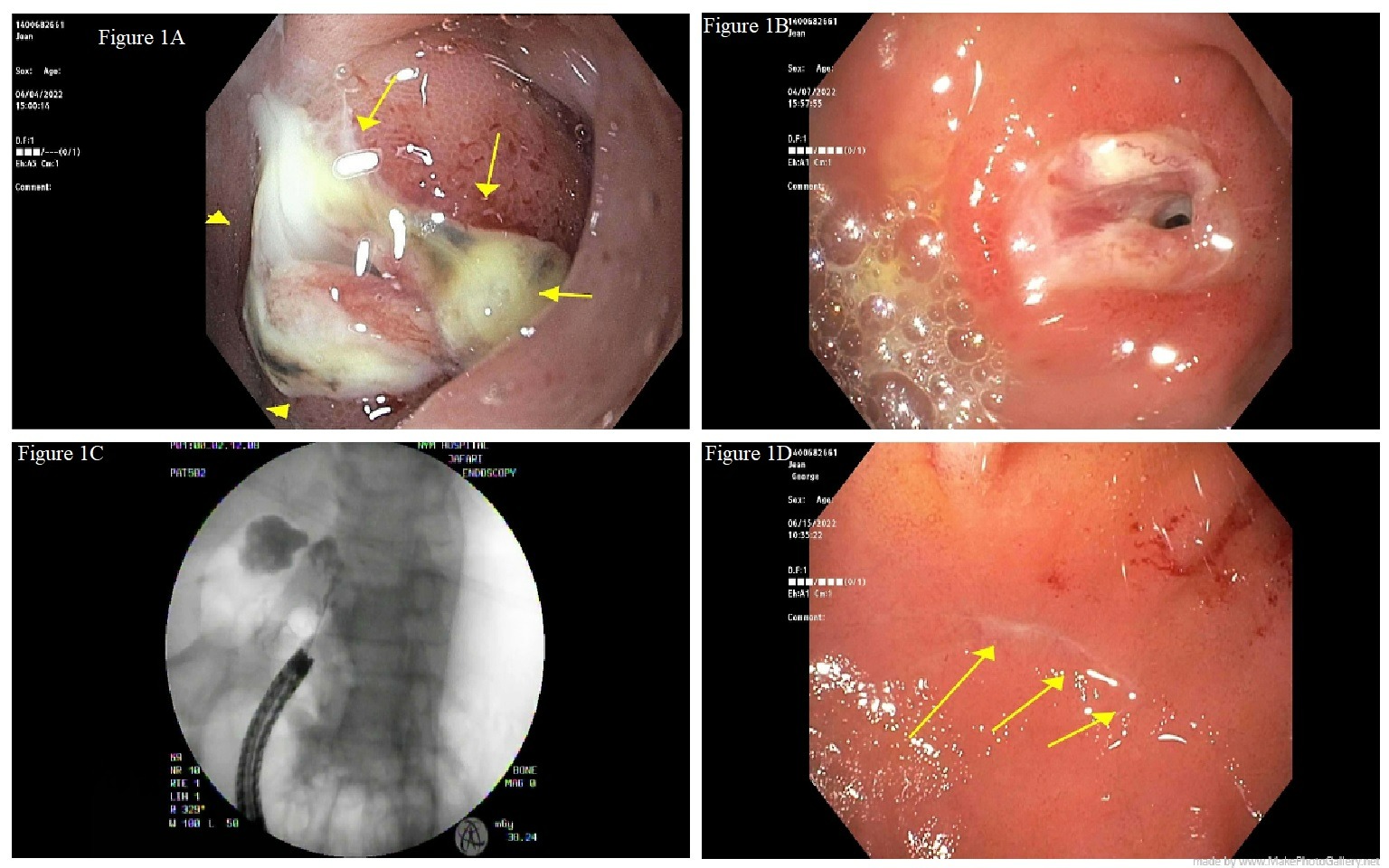
The patient was readmitted for persistent abdominal pain, weight loss and loss of appetite. On physical exam, she had epigastric tenderness. She was afebrile and lab work was normal. CT abdomen and pelvis demonstrated small bowel thickening involving the duodenal bulb and first portion of the duodenum and air within the gallbladder with mild pericholecystic inflammatory changes. An EGD performed thereafter revealed the same duodenal bulb ulcer with a likely fistula (Figure 1B); injection of contrast through the tract under fluoroscopy confirmed a fistula to the gallbladder (Figure 1C). The patient was discharged on high-dose twice daily PPI, a short course of amoxicillin and clavulanic acid. Her symptoms resolved within 8 weeks. A surveillance EGD performed to assess healing demonstrated a healed scar at the site of the prior ulcer and fistula (Figure 1D).
Discussion: Cholecystoenteric fistulas are a rare complication of gallstone disease and peptic ulcer disease, with an autopsy reported incidence rate of 0.1%-0.5%. Historically, surgical treatment is the most common treatment method for cholecystoenteric fistulas. Our case suggests that a high proton pump inhibitor dose for 8-12 weeks may be sufficient for the fistula to heal. By implementing medical management for this condition, it may be possible to avoid the morbidity and mortality associated with laparoscopic or open fistula repair.
Disclosures:
Miguel Lacayo, MD, Ezana Bekele, MD, Pratima Dibba, MD, Amar Manvar, MD, Irwin Grosman, MD. D0657 - Choledocystoduodenal Fistula Effectively Treated With a High-Dose Proton Pump Inhibitor: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Choledocystoduodenal fistulas are a rare complication of biliary or peptic ulcer disease. Approximately 91%-94% of spontaneous internal biliary fistulas are caused by stones in the biliary tract. The second most common cause is peptic ulcer. We present a case of a patient found to have a choledocystoduodenal fistula caused by peptic ulcer disease successfully treated with high-dose PPI.
Case Description/Methods: A 73-year-old female with a history of duodenitis and gastritis presented for chronic intermittent abdominal pain. Physical exam was positive for epigastric tenderness. Labs were normal. Imaging revealed a large stool burden, mildly distended gallbladder without gallstones and a normal biliary tree. She was started on a once-daily PPI and a bowel regimen. EGD was performed and demonstrated a large necrotic duodenal lesion with copious purulent drainage (Figure 1A). Gastric biopsy was negative for H. pylori.
The patient was readmitted for persistent abdominal pain, weight loss and loss of appetite. On physical exam, she had epigastric tenderness. She was afebrile and lab work was normal. CT abdomen and pelvis demonstrated small bowel thickening involving the duodenal bulb and first portion of the duodenum and air within the gallbladder with mild pericholecystic inflammatory changes. An EGD performed thereafter revealed the same duodenal bulb ulcer with a likely fistula (Figure 1B); injection of contrast through the tract under fluoroscopy confirmed a fistula to the gallbladder (Figure 1C). The patient was discharged on high-dose twice daily PPI, a short course of amoxicillin and clavulanic acid. Her symptoms resolved within 8 weeks. A surveillance EGD performed to assess healing demonstrated a healed scar at the site of the prior ulcer and fistula (Figure 1D).
Discussion: Cholecystoenteric fistulas are a rare complication of gallstone disease and peptic ulcer disease, with an autopsy reported incidence rate of 0.1%-0.5%. Historically, surgical treatment is the most common treatment method for cholecystoenteric fistulas. Our case suggests that a high proton pump inhibitor dose for 8-12 weeks may be sufficient for the fistula to heal. By implementing medical management for this condition, it may be possible to avoid the morbidity and mortality associated with laparoscopic or open fistula repair.
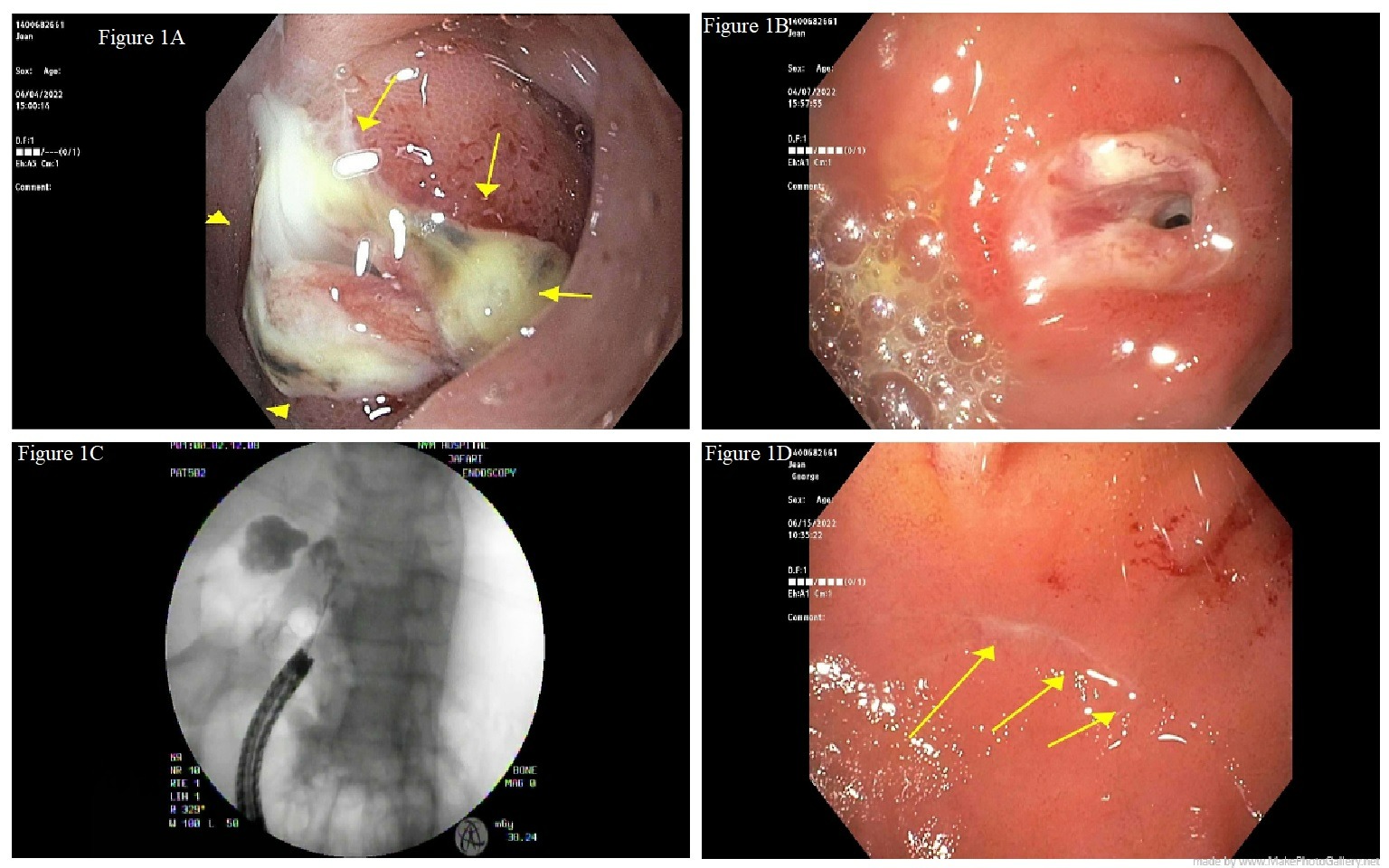
Figure: 1A. Initial EGD showing large necrotic duodenal lesion with copious purulent drainage
1B. Second EGD demonstrating duodenal bulb ulcer
1C. Fluoroscopy with contrast injection demonstrating fistula tract communication with gallbladder
1D. Follow-up EGD after treatment with high dose PPI demonstrating healed choledocystoduodenal fistula with a small residual duodenal ulcer
1B. Second EGD demonstrating duodenal bulb ulcer
1C. Fluoroscopy with contrast injection demonstrating fistula tract communication with gallbladder
1D. Follow-up EGD after treatment with high dose PPI demonstrating healed choledocystoduodenal fistula with a small residual duodenal ulcer
Disclosures:
Miguel Lacayo indicated no relevant financial relationships.
Ezana Bekele indicated no relevant financial relationships.
Pratima Dibba indicated no relevant financial relationships.
Amar Manvar indicated no relevant financial relationships.
Irwin Grosman indicated no relevant financial relationships.
Miguel Lacayo, MD, Ezana Bekele, MD, Pratima Dibba, MD, Amar Manvar, MD, Irwin Grosman, MD. D0657 - Choledocystoduodenal Fistula Effectively Treated With a High-Dose Proton Pump Inhibitor: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
