Back

Poster Session E - Tuesday Afternoon
Category: Colon
E0126 - Fibrosing Colonopathy in Chronic Alcoholic Pancreatitis: A Diagnostic Dilemma
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Muaaz Masood, MD
Medical College of Georgia at Augusta University
Augusta, GA
Presenting Author(s)
Muaaz Masood, MD1, Dariush Shahsavari, MD2, Asad Jehangir, MD3, Janet Munroe, MD1, John Erikson L. Yap, MD4, Humberto Sifuentes, MD5
1Medical College of Georgia at Augusta University, Augusta, GA; 2Medical College of Georgia - Augusta University, Augusta, GA; 3Augusta University, Augusta, GA; 4Augusta University Medical College of Georiga, Augusta, GA; 5Augusta University Medical College of Georgia, Augusta, GA
Introduction: Fibrosing colonopathy (FC) is a rare entity that has been associated with high-dose pancreatic enzyme replacement therapy (PERT) and has been mostly reported in patients with cystic fibrosis. We present a case of chronic alcoholic pancreatitis and FC that eluded diagnosis for 4 years resulting in multiple endoscopic interventions.
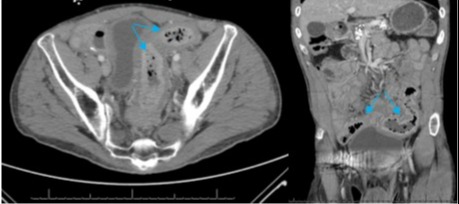
Case Description/Methods: A 47-year-old male with a history of substance abuse and chronic alcoholic pancreatitis presented with 1.5 days of lower abdominal pain, nausea and vomiting. He reported chronic watery diarrhea up to 5 times/day and lost 20 kg within 1 year. His current weight was 64 kg. Patient was on pancrelipase 24,000 units thrice daily, but he was intermittently non-adherent with PERT due to socioeconomic issues. He had 21 prior CT scans suggestive of colitis for which he underwent 5 lower endoscopic evaluations in the span of 4 years. Random colonic biopsies from these endoscopies were all histologically normal. Work-up for infectious, celiac, thyroid and inflammatory bowel diseases was unremarkable. Fecal elastase was undetectable. Vitamins A, D and E levels were low. After a second careful review of all prior images with radiologist, there was evidence of chronic, colonic wall thickening without inflammation consistent with FC. After excluding other pathology, exocrine pancreatic insufficiency was the likely etiology of his symptoms. The patient was continued on the current dose of PERT and nutrition consultation was recommended.
Discussion: FC is a long segment colonic disease characterized by a gradual, fusiform stenosis of the lumen resulting from submucosal fibrosis. The exact pathogenesis remains unknown, but it has been associated with high doses of PERT and compounds in the enteric-coated material. FC may occur months to years after the initiation of high-dose PERT. Interestingly, our patient was on PERT for 5 years and was prescribed an appropriate dose. FC commonly manifests as abdominal pain, diarrhea, hematochezia and, in some cases, small bowel obstruction. Prior intestinal surgery is a possible risk factor for FC. On endoscopy, a loss of haustral pattern or “cobblestone” colonic mucosa may be seen. While a full thickness colonic resection is the gold standard for diagnosis, FC was diagnosed in our case based on clinical and radiologic data after exclusion of other pathology. Management of FC involves avoidance of high doses of PERT ( >10,000 units/kg/day). Surgical resection of the colon is reserved for refractory cases
Disclosures:
Muaaz Masood, MD1, Dariush Shahsavari, MD2, Asad Jehangir, MD3, Janet Munroe, MD1, John Erikson L. Yap, MD4, Humberto Sifuentes, MD5. E0126 - Fibrosing Colonopathy in Chronic Alcoholic Pancreatitis: A Diagnostic Dilemma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Medical College of Georgia at Augusta University, Augusta, GA; 2Medical College of Georgia - Augusta University, Augusta, GA; 3Augusta University, Augusta, GA; 4Augusta University Medical College of Georiga, Augusta, GA; 5Augusta University Medical College of Georgia, Augusta, GA
Introduction: Fibrosing colonopathy (FC) is a rare entity that has been associated with high-dose pancreatic enzyme replacement therapy (PERT) and has been mostly reported in patients with cystic fibrosis. We present a case of chronic alcoholic pancreatitis and FC that eluded diagnosis for 4 years resulting in multiple endoscopic interventions.
Case Description/Methods: A 47-year-old male with a history of substance abuse and chronic alcoholic pancreatitis presented with 1.5 days of lower abdominal pain, nausea and vomiting. He reported chronic watery diarrhea up to 5 times/day and lost 20 kg within 1 year. His current weight was 64 kg. Patient was on pancrelipase 24,000 units thrice daily, but he was intermittently non-adherent with PERT due to socioeconomic issues. He had 21 prior CT scans suggestive of colitis for which he underwent 5 lower endoscopic evaluations in the span of 4 years. Random colonic biopsies from these endoscopies were all histologically normal. Work-up for infectious, celiac, thyroid and inflammatory bowel diseases was unremarkable. Fecal elastase was undetectable. Vitamins A, D and E levels were low. After a second careful review of all prior images with radiologist, there was evidence of chronic, colonic wall thickening without inflammation consistent with FC. After excluding other pathology, exocrine pancreatic insufficiency was the likely etiology of his symptoms. The patient was continued on the current dose of PERT and nutrition consultation was recommended.
Discussion: FC is a long segment colonic disease characterized by a gradual, fusiform stenosis of the lumen resulting from submucosal fibrosis. The exact pathogenesis remains unknown, but it has been associated with high doses of PERT and compounds in the enteric-coated material. FC may occur months to years after the initiation of high-dose PERT. Interestingly, our patient was on PERT for 5 years and was prescribed an appropriate dose. FC commonly manifests as abdominal pain, diarrhea, hematochezia and, in some cases, small bowel obstruction. Prior intestinal surgery is a possible risk factor for FC. On endoscopy, a loss of haustral pattern or “cobblestone” colonic mucosa may be seen. While a full thickness colonic resection is the gold standard for diagnosis, FC was diagnosed in our case based on clinical and radiologic data after exclusion of other pathology. Management of FC involves avoidance of high doses of PERT ( >10,000 units/kg/day). Surgical resection of the colon is reserved for refractory cases
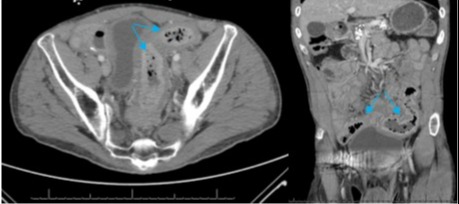
Figure: Panel 1. Axial view (left) and coronal view (right) of an abdominopelvic computed tomography scan with intravenous contrast demonstrating colonic wall thickening of the mid and distal sigmoid colon (blue arrows).
Disclosures:
Muaaz Masood indicated no relevant financial relationships.
Dariush Shahsavari indicated no relevant financial relationships.
Asad Jehangir indicated no relevant financial relationships.
Janet Munroe indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Humberto Sifuentes indicated no relevant financial relationships.
Muaaz Masood, MD1, Dariush Shahsavari, MD2, Asad Jehangir, MD3, Janet Munroe, MD1, John Erikson L. Yap, MD4, Humberto Sifuentes, MD5. E0126 - Fibrosing Colonopathy in Chronic Alcoholic Pancreatitis: A Diagnostic Dilemma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
