Back

Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0315 - Abscess-Enteric Fistula of Failed Kidney Transplant Presenting With Gastrointestinal Bleeding
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Bianca Di Cocco, MD
New York-Presbyterian/Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Bianca Di Cocco, MD1, Preston Atteberry, MD2, David Wan, MD2
1New York-Presbyterian/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Lower gastrointestinal (GI) bleeding is a common occurrence, with the vast majority of cases being due to diverticula, vascular ectasias, cancers, and hemorrhoids. In rare cases, a large vessel can form a fistula with the GI tract, causing bleeding. We present a case where an abscess surrounding a failed transplant kidney eroded into the external iliac vein and presented as a slow lower GI bleed.
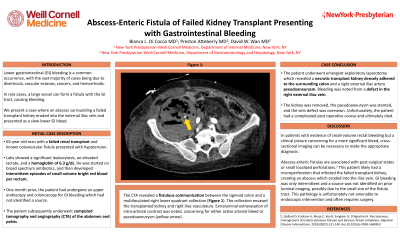
Case Description/Methods: A 65-year-old man with a failed renal transplant and known colovesicular fistula presented with hypotension. Labs showed a significant leukocytosis, an elevated lactate, and a hemoglobin of 6.3 g/dL. He was started on broad spectrum antibiotics, and then developed intermittent episodes of small-volume bright red blood per rectum. The patient had an upper endoscopy and colonoscopy one month prior for GI bleeding which had not identified a source. Computed tomography angiography of the abdomen and pelvis revealed a fistulous communication between the sigmoid colon and a multiloculated right lower quadrant collection (Figure 1). The collection encased the transplanted kidney and right iliac vasculature. Extraluminal extravasation of intra-arterial contrast was noted, concerning for either active arterial bleed or pseudoaneurysm. The patient underwent emergent exploratory laparotomy which revealed a necrotic transplant kidney densely adhered to the surrounding colon and a right external iliac artery pseudoaneurysm. Bleeding was noted from a defect in the right external iliac vein. The kidney was removed, the pseudoaneurysm was stented, and the vein defect was oversewn. Unfortunately, the patient had a complicated post operative course and died.
Discussion: In patients with evidence of small-volume rectal bleeding but a clinical picture concerning for a more significant bleed, cross-sectional imaging can be necessary to make the appropriate diagnosis. In this case, imaging identified the abscess-enteric fistula, and laparoscopy revealed that the bleeding was due to a defect in the iliac vein. Abscess-enteric fistulas are associated with post-surgical states or small localized perforations. This patient likely developed a microperforation that infected the failed transplant kidney, creating an abscess which eroded into the iliac vein. GI bleeding was only intermittent and a source was not identified on prior luminal imaging, possibly due to the small size of the fistula tract. This pathology is unfortunately not amenable to endoscopic intervention and often requires surgery.

Disclosures:
Bianca Di Cocco, MD1, Preston Atteberry, MD2, David Wan, MD2. E0315 - Abscess-Enteric Fistula of Failed Kidney Transplant Presenting With Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York-Presbyterian/Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY
Introduction: Lower gastrointestinal (GI) bleeding is a common occurrence, with the vast majority of cases being due to diverticula, vascular ectasias, cancers, and hemorrhoids. In rare cases, a large vessel can form a fistula with the GI tract, causing bleeding. We present a case where an abscess surrounding a failed transplant kidney eroded into the external iliac vein and presented as a slow lower GI bleed.
Case Description/Methods: A 65-year-old man with a failed renal transplant and known colovesicular fistula presented with hypotension. Labs showed a significant leukocytosis, an elevated lactate, and a hemoglobin of 6.3 g/dL. He was started on broad spectrum antibiotics, and then developed intermittent episodes of small-volume bright red blood per rectum. The patient had an upper endoscopy and colonoscopy one month prior for GI bleeding which had not identified a source. Computed tomography angiography of the abdomen and pelvis revealed a fistulous communication between the sigmoid colon and a multiloculated right lower quadrant collection (Figure 1). The collection encased the transplanted kidney and right iliac vasculature. Extraluminal extravasation of intra-arterial contrast was noted, concerning for either active arterial bleed or pseudoaneurysm. The patient underwent emergent exploratory laparotomy which revealed a necrotic transplant kidney densely adhered to the surrounding colon and a right external iliac artery pseudoaneurysm. Bleeding was noted from a defect in the right external iliac vein. The kidney was removed, the pseudoaneurysm was stented, and the vein defect was oversewn. Unfortunately, the patient had a complicated post operative course and died.
Discussion: In patients with evidence of small-volume rectal bleeding but a clinical picture concerning for a more significant bleed, cross-sectional imaging can be necessary to make the appropriate diagnosis. In this case, imaging identified the abscess-enteric fistula, and laparoscopy revealed that the bleeding was due to a defect in the iliac vein. Abscess-enteric fistulas are associated with post-surgical states or small localized perforations. This patient likely developed a microperforation that infected the failed transplant kidney, creating an abscess which eroded into the iliac vein. GI bleeding was only intermittent and a source was not identified on prior luminal imaging, possibly due to the small size of the fistula tract. This pathology is unfortunately not amenable to endoscopic intervention and often requires surgery.

Figure: Computed tomography angiography of the abdomen and pelvis with a multiloculated right lower quadrant collection encasing a transplanted kidney and right iliac vasculature.
Disclosures:
Bianca Di Cocco indicated no relevant financial relationships.
Preston Atteberry indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Bianca Di Cocco, MD1, Preston Atteberry, MD2, David Wan, MD2. E0315 - Abscess-Enteric Fistula of Failed Kidney Transplant Presenting With Gastrointestinal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
