Back

Poster Session E - Tuesday Afternoon
Category: GI Bleeding
E0320 - CMV Ileitis: An Unusual but Important Cause of Acute GI Bleeding in COVID-19 Patients on ECMO
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Samantha Storti, DO
Advocate Christ Medical Center
Oak Lawn, IL
Presenting Author(s)
Samantha Storti, DO, Sylvia Chlebek, DO, Hareth Raddawi, MD
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Cytomegalovirus (CMV) can affect many organ systems including the gastrointestinal tract. There are few cases that report ileal involvement due to CMV in patients with COVID-19 on ECMO. To our knowledge, these are two of the first documented cases of hemorrhagic CMV ileitis in patients with COVID- 19 who received extracorporeal membrane oxygenation (ECMO).
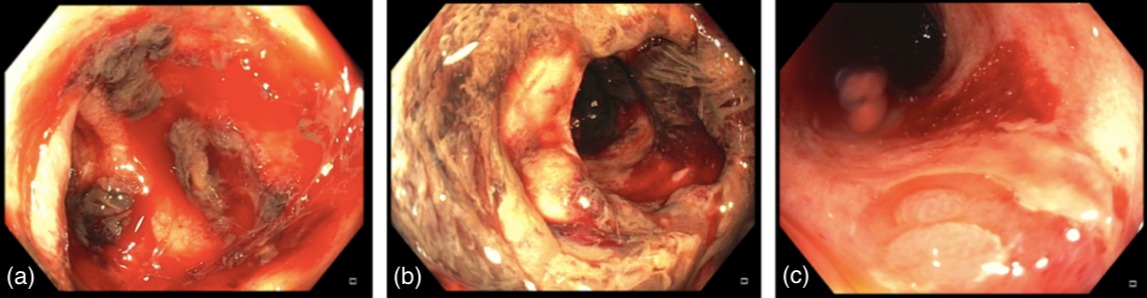
Case Description/Methods: Case 1: A 55-year-old male with hypertension, asthma, gastro-esophageal reflux disease and gout was hospitalized for worsening acute hypoxemic respiratory failure secondary to COVID-19 requiring ECMO. Progressive lactic acidosis raised concerns for bowel ischemia. Flexible sigmoidoscopy revealed large amounts of blood and clots, suggestive of colonic ischemia in the rectosigmoid region. The patient developed further gastrointestinal hemorrhage warranting colonoscopy and ileoscopy which revealed areas of extensive ulceration and active bleeding within the terminal ileum (Figure 1a, 1b). Biopsies were positive for CMV and ganciclovir was initiated. Despite medical intervention, the patient succumbed to multiorgan failure and expired.
Case 2: A 62-year-old male with hypertension and obesity was transferred to our facility for ECMO in the setting of worsening acute hypoxemic respiratory failure secondary to COVID-19. An episode of melena prompted endoscopic evaluation. EGD revealed ulcerations in the body of the stomach without active bleeding or visible vessels. The patient developed rectal bleeding and colonoscopy revealed moderate amounts of fresh and clotted blood throughout the colon with areas of severe ulcerations in the ileum (Figure 1c). Ganciclovir was started empirically and biopsies subsequently confirmed diagnosis of CMV. The patient developed multisystem organ failure and expired.
Discussion: CMV classically involves the esophagus and colon in those who are immunocompromised. These two cases demonstrate atypical presentations of CMV. Both patients had ileal involvement and neither had a known history of immunocompromise, including negative HIV testing. Earlier in their hospitalizations, both patients received high dose steroids and remdesivir as part of treatment for COVID-19. This raises concern that transient immunosuppression may have led to primary CMV infection or reactivation of previously dormant CMV. Because mortality is high in this population, ileal disease secondary to CMV should be considered as a cause of gastrointestinal hemorrhage in order for therapy to be initiated early.
Disclosures:
Samantha Storti, DO, Sylvia Chlebek, DO, Hareth Raddawi, MD. E0320 - CMV Ileitis: An Unusual but Important Cause of Acute GI Bleeding in COVID-19 Patients on ECMO, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Advocate Christ Medical Center, Oak Lawn, IL
Introduction: Cytomegalovirus (CMV) can affect many organ systems including the gastrointestinal tract. There are few cases that report ileal involvement due to CMV in patients with COVID-19 on ECMO. To our knowledge, these are two of the first documented cases of hemorrhagic CMV ileitis in patients with COVID- 19 who received extracorporeal membrane oxygenation (ECMO).
Case Description/Methods: Case 1: A 55-year-old male with hypertension, asthma, gastro-esophageal reflux disease and gout was hospitalized for worsening acute hypoxemic respiratory failure secondary to COVID-19 requiring ECMO. Progressive lactic acidosis raised concerns for bowel ischemia. Flexible sigmoidoscopy revealed large amounts of blood and clots, suggestive of colonic ischemia in the rectosigmoid region. The patient developed further gastrointestinal hemorrhage warranting colonoscopy and ileoscopy which revealed areas of extensive ulceration and active bleeding within the terminal ileum (Figure 1a, 1b). Biopsies were positive for CMV and ganciclovir was initiated. Despite medical intervention, the patient succumbed to multiorgan failure and expired.
Case 2: A 62-year-old male with hypertension and obesity was transferred to our facility for ECMO in the setting of worsening acute hypoxemic respiratory failure secondary to COVID-19. An episode of melena prompted endoscopic evaluation. EGD revealed ulcerations in the body of the stomach without active bleeding or visible vessels. The patient developed rectal bleeding and colonoscopy revealed moderate amounts of fresh and clotted blood throughout the colon with areas of severe ulcerations in the ileum (Figure 1c). Ganciclovir was started empirically and biopsies subsequently confirmed diagnosis of CMV. The patient developed multisystem organ failure and expired.
Discussion: CMV classically involves the esophagus and colon in those who are immunocompromised. These two cases demonstrate atypical presentations of CMV. Both patients had ileal involvement and neither had a known history of immunocompromise, including negative HIV testing. Earlier in their hospitalizations, both patients received high dose steroids and remdesivir as part of treatment for COVID-19. This raises concern that transient immunosuppression may have led to primary CMV infection or reactivation of previously dormant CMV. Because mortality is high in this population, ileal disease secondary to CMV should be considered as a cause of gastrointestinal hemorrhage in order for therapy to be initiated early.
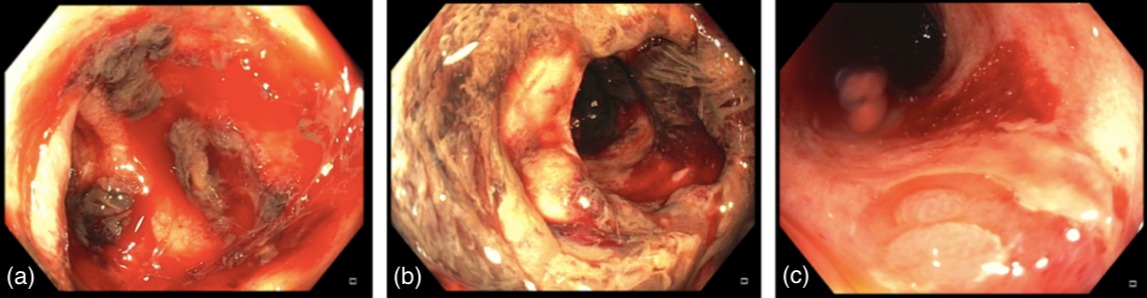
Figure: Figure 1a-c: Colonoscopic imaging of mucosal abnormalities of the terminal ileum in patients with CMV. The following figures demonstrate the macroscopic changes to the gastrointestinal tract in those with severe CMV infection. Figure 1a and 1b show severe mucosal ulceration with active bleeding and old blood within the termite ileum. Fgure 1c shows focal ulcerations with visible vessels and fresh blood within the terminal ileum.
Disclosures:
Samantha Storti indicated no relevant financial relationships.
Sylvia Chlebek indicated no relevant financial relationships.
Hareth Raddawi indicated no relevant financial relationships.
Samantha Storti, DO, Sylvia Chlebek, DO, Hareth Raddawi, MD. E0320 - CMV Ileitis: An Unusual but Important Cause of Acute GI Bleeding in COVID-19 Patients on ECMO, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

