Back

Poster Session D - Tuesday Morning
Category: Stomach
D0726 - Primary Gastric Tuberculosis Without Pulmonary Involvement Presenting as Chronic Reflux With Anemia
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Alejandro Villanueva, MD
Norwalk Hospital
Norwalk, CT
Presenting Author(s)
Alejandro Villanueva, MD1, Triston Berger, MD1, Naveen Anand, MD1, Vikram Anand, MD2
1Norwalk Hospital, Norwalk, CT; 2John Peter Smith Hospital, Fort Worth, TX
Introduction: Gastrointestinal (GI) tuberculosis (TB) accounts for only 1-3% of TB cases worldwide. Of these GI cases, the ileocecal region is the most affected site. Gastric Tuberculosis (GTB) only accounts for 1-2% of GI TB. When present, GTB is typically seen in conjunction with pulmonary tuberculosis or associated with an immunodeficient state. Primary, isolated GTB in the immunocompetent is particularly rare. When present, GTB commonly presents as gastric outlet obstruction but can also have symptoms that mimic peptic ulcer disease or malignancy. The diagnosis requires biopsy showing caseating granulomas or the presence of acid-fast bacilli. We present a case of isolated GTB in routine workup of a patient with chronic anemia.
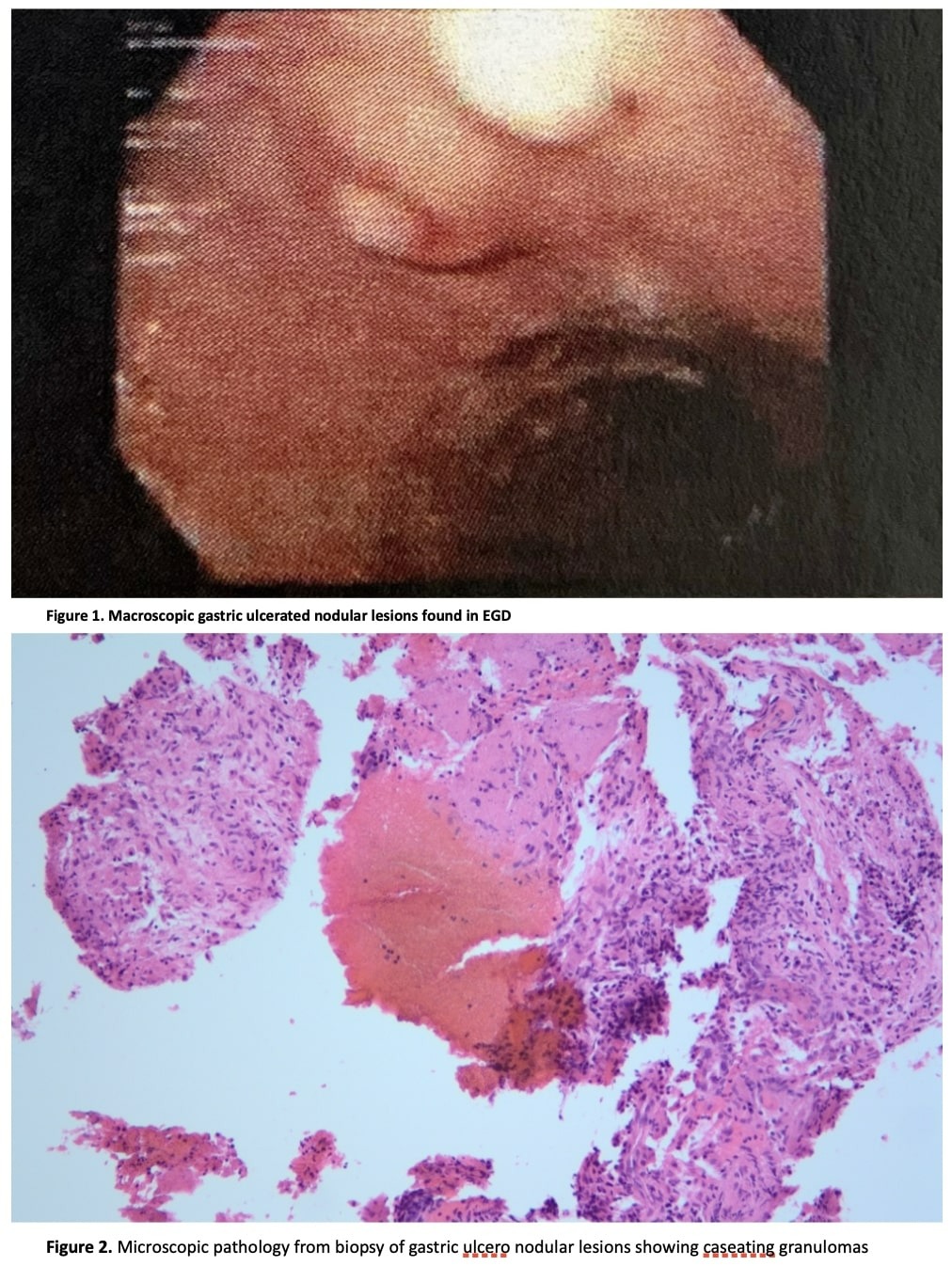
Case Description/Methods: 60-year-old Honduran male with history of Parkinson’s disease presented for evaluation of constipation, reflux, and chronic anemia. He underwent endoscopy and colonoscopy revealing several gastric submucosal nodules as well as a duodenal ulceration (Figure 1). He subsequently had endoscopic ultrasound with biopsy for two of these nodules which was remarkable for chronic granulomatous inflammation with necrosis and inflamed fibrous tissue, and caseating granulomatous inflammation respectively (Figure 2). Acid-fast stain showed an indeterminant rod-shaped organism. He tested negative for TB polymerase chain reaction but positive for QuantiFERON-TB. There was concern for disseminated TB and CT scan chest/abdomen/pelvis was done which did not show any suspicious lesions. Gastric TB was diagnosed, and the patient received anti-tubercular treatment.
Discussion: Although rare, clinicians should be suspicious of GTB in patients native to endemic areas presenting with symptoms reflecting gastric outlet obstruction, peptic ulcer disease, malignancy, or in the workup of chronic anemia. The lack of pulmonary involvement as seen in this case makes it particularly challenging to identify. The routes of infection of the gastric tissue include hematogenous spread, extension from neighboring TB lesion, or direct infection of the mucosa. The rarity of GTB can be attributed to the bactericidal properties of gastric acid and lack of significant lymphoid tissue in the gastric wall. The gastric mucosal barrier also plays a part in preventing migration into the tissue. Given the chronic reflux in this patient, it is possible he had gastritis and erosion of the barrier facilitating infection. Once diagnosed, patients respond well to anti-tubercular treatment.
Disclosures:
Alejandro Villanueva, MD1, Triston Berger, MD1, Naveen Anand, MD1, Vikram Anand, MD2. D0726 - Primary Gastric Tuberculosis Without Pulmonary Involvement Presenting as Chronic Reflux With Anemia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Norwalk Hospital, Norwalk, CT; 2John Peter Smith Hospital, Fort Worth, TX
Introduction: Gastrointestinal (GI) tuberculosis (TB) accounts for only 1-3% of TB cases worldwide. Of these GI cases, the ileocecal region is the most affected site. Gastric Tuberculosis (GTB) only accounts for 1-2% of GI TB. When present, GTB is typically seen in conjunction with pulmonary tuberculosis or associated with an immunodeficient state. Primary, isolated GTB in the immunocompetent is particularly rare. When present, GTB commonly presents as gastric outlet obstruction but can also have symptoms that mimic peptic ulcer disease or malignancy. The diagnosis requires biopsy showing caseating granulomas or the presence of acid-fast bacilli. We present a case of isolated GTB in routine workup of a patient with chronic anemia.
Case Description/Methods: 60-year-old Honduran male with history of Parkinson’s disease presented for evaluation of constipation, reflux, and chronic anemia. He underwent endoscopy and colonoscopy revealing several gastric submucosal nodules as well as a duodenal ulceration (Figure 1). He subsequently had endoscopic ultrasound with biopsy for two of these nodules which was remarkable for chronic granulomatous inflammation with necrosis and inflamed fibrous tissue, and caseating granulomatous inflammation respectively (Figure 2). Acid-fast stain showed an indeterminant rod-shaped organism. He tested negative for TB polymerase chain reaction but positive for QuantiFERON-TB. There was concern for disseminated TB and CT scan chest/abdomen/pelvis was done which did not show any suspicious lesions. Gastric TB was diagnosed, and the patient received anti-tubercular treatment.
Discussion: Although rare, clinicians should be suspicious of GTB in patients native to endemic areas presenting with symptoms reflecting gastric outlet obstruction, peptic ulcer disease, malignancy, or in the workup of chronic anemia. The lack of pulmonary involvement as seen in this case makes it particularly challenging to identify. The routes of infection of the gastric tissue include hematogenous spread, extension from neighboring TB lesion, or direct infection of the mucosa. The rarity of GTB can be attributed to the bactericidal properties of gastric acid and lack of significant lymphoid tissue in the gastric wall. The gastric mucosal barrier also plays a part in preventing migration into the tissue. Given the chronic reflux in this patient, it is possible he had gastritis and erosion of the barrier facilitating infection. Once diagnosed, patients respond well to anti-tubercular treatment.
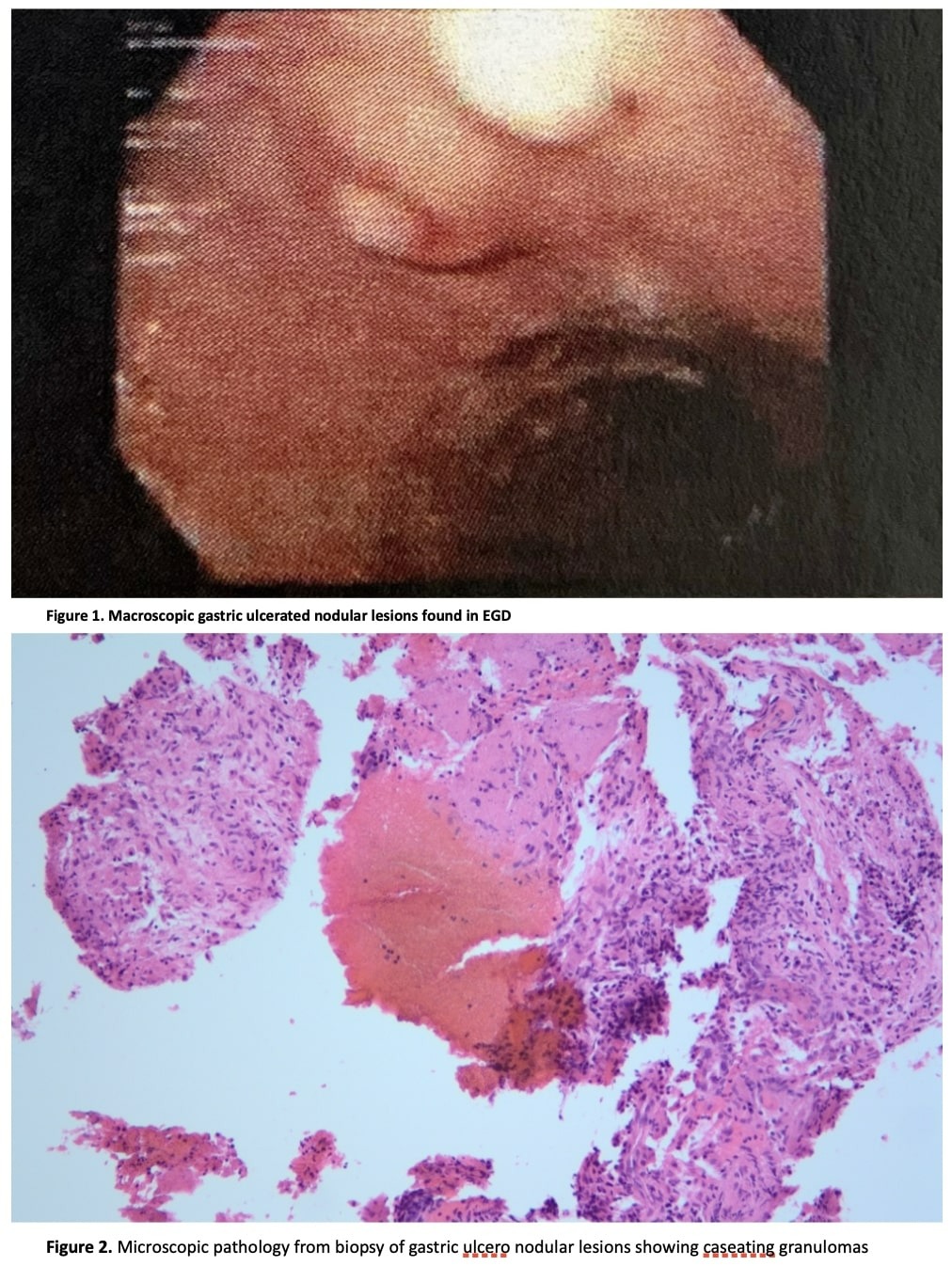
Figure: Figure 1. Macroscopic gastric ulcerated nodular lesions found in EGD
igure 2. Microscopic pathology from biopsy of gastric ulcero nodular lesions showing caseating granulomas
igure 2. Microscopic pathology from biopsy of gastric ulcero nodular lesions showing caseating granulomas
Disclosures:
Alejandro Villanueva indicated no relevant financial relationships.
Triston Berger indicated no relevant financial relationships.
Naveen Anand indicated no relevant financial relationships.
Vikram Anand indicated no relevant financial relationships.
Alejandro Villanueva, MD1, Triston Berger, MD1, Naveen Anand, MD1, Vikram Anand, MD2. D0726 - Primary Gastric Tuberculosis Without Pulmonary Involvement Presenting as Chronic Reflux With Anemia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
