Back

Poster Session B - Monday Morning
Category: Stomach
B0709 - Pyogenic Granuloma Found in the Duodenum: A Rare Etiology
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Herman Suga, DO
Jefferson Health New Jersey
Turnersville, NJ
Presenting Author(s)
Herman Suga, DO1, Neethi Dasu, DO2, Charles Yang, DO3, Brian Blair, DO4, C. Jonathan Foster, DO5
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health New Jersey, Voorhees, NJ; 3Jefferson Health New Jersey, Stratford, NJ; 4Jefferson Health New Jersey, Cherry HIll, NJ; 5Jefferson Health New Jersey, Cherry Hill, NJ
Introduction: Pyogenic granuloma (PG) is a benign growth of capillary blood vessels arranged in lobular fashion. While infection, trauma and hormones are implicated as causes, the exact etiology is unknown. PG is commonly found on the skin and oral mucosa but PG occurrences in the duodenum are extremely rare. We present an unusual case of a duodenal PG as a cause of anemia and gastrointestinal (GI) bleeding in a 68 year old female.
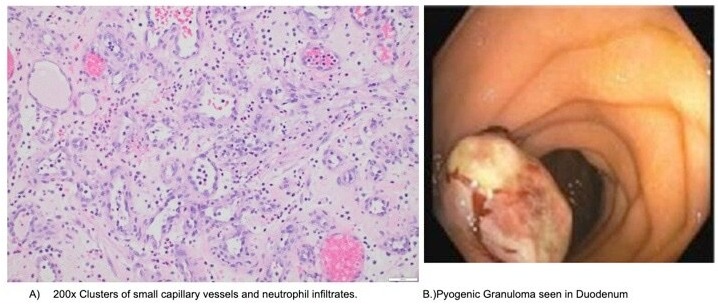
Case Description/Methods: A 68-year-old female with history of laparoscopic adjustable gastric banding presented for evaluation of fatigue and shortness of breath. She was found to have microcytic anemia with a decline of hemoglobin 13.3gm/dL to 8.5 gm/dLwithin one year. She underwent bi-directional endoscopic evaluation which revealed normal duodenum, esophagitis, gastritis, and evidence of laparoscopic revision surgery. Biopsies were negative for Celiac disease and Heliobacter pylori. Colonoscopy and Small bowel capsule endoscopy revealed no source of bleeding. Push enteroscopy demonstrated a 15mm polyp in the third part of the duodenum. Biopsies of the duodenal polyp showed granulation tissue without small intestinal mucosa. Endoscopic mucosal resection (EMR) of the polyp with argon plasma coagulation (APC) of the edges was completed. Pathology revealed polypoid granulation tissue with surface ulceration and acute inflammation consistent with pyogenic granuloma (PG) of the duodenum. The patient was instructed to return for follow-up EGD in six months.
Discussion: An immunohistochemical stain (CD3) of the PG revealed scattered T-cells. PillCam footage was reviewed and confirmed that this lesion was not previously present. While the pathogenesis of PG is unknown, theories include imbalance of angiogenesis factors and mechanical trauma. Furthermore, very few cases of duodenal PG have been described in the literature. Diagnostic workup of PG in the GI tract has not yet been agreed upon but commonly utilized techniques include EGD, PillCam Endoscopy, push enteroscopy, and double balloon enteroscopy. Imaging that detects the readily hemorrhaging papule in conjunction with biopsy is ideal. Treatment options include EMR, laser ablation or surgery. This case is important because it highlights an extremely rare cause of gastrointestinal bleeding. Diagnosis can be difficult, and it is important for practitioners to be vigilant in recognizing this disease entity because PG can hemorrhage and lead to profuse GI bleeding.
Disclosures:
Herman Suga, DO1, Neethi Dasu, DO2, Charles Yang, DO3, Brian Blair, DO4, C. Jonathan Foster, DO5. B0709 - Pyogenic Granuloma Found in the Duodenum: A Rare Etiology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jefferson Health New Jersey, Turnersville, NJ; 2Jefferson Health New Jersey, Voorhees, NJ; 3Jefferson Health New Jersey, Stratford, NJ; 4Jefferson Health New Jersey, Cherry HIll, NJ; 5Jefferson Health New Jersey, Cherry Hill, NJ
Introduction: Pyogenic granuloma (PG) is a benign growth of capillary blood vessels arranged in lobular fashion. While infection, trauma and hormones are implicated as causes, the exact etiology is unknown. PG is commonly found on the skin and oral mucosa but PG occurrences in the duodenum are extremely rare. We present an unusual case of a duodenal PG as a cause of anemia and gastrointestinal (GI) bleeding in a 68 year old female.
Case Description/Methods: A 68-year-old female with history of laparoscopic adjustable gastric banding presented for evaluation of fatigue and shortness of breath. She was found to have microcytic anemia with a decline of hemoglobin 13.3gm/dL to 8.5 gm/dLwithin one year. She underwent bi-directional endoscopic evaluation which revealed normal duodenum, esophagitis, gastritis, and evidence of laparoscopic revision surgery. Biopsies were negative for Celiac disease and Heliobacter pylori. Colonoscopy and Small bowel capsule endoscopy revealed no source of bleeding. Push enteroscopy demonstrated a 15mm polyp in the third part of the duodenum. Biopsies of the duodenal polyp showed granulation tissue without small intestinal mucosa. Endoscopic mucosal resection (EMR) of the polyp with argon plasma coagulation (APC) of the edges was completed. Pathology revealed polypoid granulation tissue with surface ulceration and acute inflammation consistent with pyogenic granuloma (PG) of the duodenum. The patient was instructed to return for follow-up EGD in six months.
Discussion: An immunohistochemical stain (CD3) of the PG revealed scattered T-cells. PillCam footage was reviewed and confirmed that this lesion was not previously present. While the pathogenesis of PG is unknown, theories include imbalance of angiogenesis factors and mechanical trauma. Furthermore, very few cases of duodenal PG have been described in the literature. Diagnostic workup of PG in the GI tract has not yet been agreed upon but commonly utilized techniques include EGD, PillCam Endoscopy, push enteroscopy, and double balloon enteroscopy. Imaging that detects the readily hemorrhaging papule in conjunction with biopsy is ideal. Treatment options include EMR, laser ablation or surgery. This case is important because it highlights an extremely rare cause of gastrointestinal bleeding. Diagnosis can be difficult, and it is important for practitioners to be vigilant in recognizing this disease entity because PG can hemorrhage and lead to profuse GI bleeding.
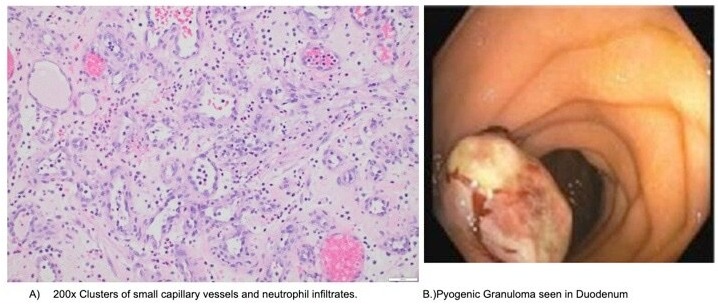
Figure: Pyogenic Granuloma seen on histology and gross image
Disclosures:
Herman Suga indicated no relevant financial relationships.
Neethi Dasu indicated no relevant financial relationships.
Charles Yang indicated no relevant financial relationships.
Brian Blair indicated no relevant financial relationships.
C. Jonathan Foster indicated no relevant financial relationships.
Herman Suga, DO1, Neethi Dasu, DO2, Charles Yang, DO3, Brian Blair, DO4, C. Jonathan Foster, DO5. B0709 - Pyogenic Granuloma Found in the Duodenum: A Rare Etiology, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
