Back

Poster Session E - Tuesday Afternoon
Category: IBD
E0403 - Opioid Exposure in Hospitalized Patients With Inflammatory Bowel Disease, in a Community Setting
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- AB
Andrew Bensinger, DO
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Andrew Bensinger, DO, Tess Petersen, MD, Julianna Tantum, DO, Adam Kaufman, MD
Lankenau Medical Center, Wynnewood, PA
Introduction: Patients with inflammatory bowel disease (Crohn’s Disease and Ulcerative Colitis) commonly present to the hospital with disease flares,characterized by changes in stool habits with abdominal, pelvic, and extra-intestinal pain. It is well established that opioid use ininflammatory bowel disease patients is associated with increased rates of infections and increased mortality. Despite this, patients with IBD typically receive opiate therapy in increasing quantities during hospitalizations to treat their pain.
We evaluated the degree of inpatient opiate use in IBD patients admitted in a community hospital setting to establish the degree of opportunity for quality improvement.
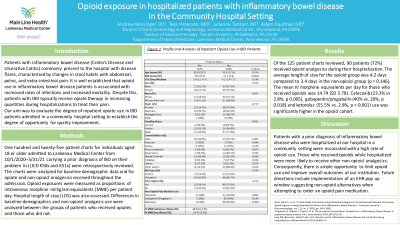
Methods: One hundred and twenty-five patient charts for individuals aged 18 or older admitted to Lankenau Medical Center from 10/1/2020 – 3/31/21 carrying a prior diagnosis of IBD on their problem list (ICD K50x and K51x) were retrospectively reviewed. The charts were analyzed for baseline demographic data and for opiate and non-opioid analgesics received throughout the admission. Opioid exposures were measured as proportions of intravenous morphine milligram equivalents (MME) per patient day. Hospital length of stay (LOS) was also assessed. Differences in baseline demographics and non-opioid analgesic use were analyzed between the groups of patients who received opiates and those who did not.
Results: Of the 125 patient charts reviewed, 90 patients (72%) received opioid analgesics during their hospitalization. The average length of stay for the opioid group was 4.2 days compared to 3.4 days in the non-opioid group (p = 0.146). The mean IV morphine equivalents per day for those who received opioids was 14.74. Celecoxib (23.3% vs 2.8%, p 0.005), gabapentin/pregabalin (40% vs. 20%, p 0.018) and ketorolac (55.5% vs. 2.8%, p < 0.001) use was significantly higher in the opioid cohort.
Discussion: Patients with a prior diagnosis of inflammatory bowel disease who were hospitalized at our hospital in a community setting were associated with a high rate of opioid use. Those who received opioids while hospitalized were more likely to receive other non-opioid analgesics. Consequently, there is ample opportunity to limit opioid use and improve overall outcomes at our institution.
Disclosures:
Andrew Bensinger, DO, Tess Petersen, MD, Julianna Tantum, DO, Adam Kaufman, MD. E0403 - Opioid Exposure in Hospitalized Patients With Inflammatory Bowel Disease, in a Community Setting, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Patients with inflammatory bowel disease (Crohn’s Disease and Ulcerative Colitis) commonly present to the hospital with disease flares,characterized by changes in stool habits with abdominal, pelvic, and extra-intestinal pain. It is well established that opioid use ininflammatory bowel disease patients is associated with increased rates of infections and increased mortality. Despite this, patients with IBD typically receive opiate therapy in increasing quantities during hospitalizations to treat their pain.
We evaluated the degree of inpatient opiate use in IBD patients admitted in a community hospital setting to establish the degree of opportunity for quality improvement.
Methods: One hundred and twenty-five patient charts for individuals aged 18 or older admitted to Lankenau Medical Center from 10/1/2020 – 3/31/21 carrying a prior diagnosis of IBD on their problem list (ICD K50x and K51x) were retrospectively reviewed. The charts were analyzed for baseline demographic data and for opiate and non-opioid analgesics received throughout the admission. Opioid exposures were measured as proportions of intravenous morphine milligram equivalents (MME) per patient day. Hospital length of stay (LOS) was also assessed. Differences in baseline demographics and non-opioid analgesic use were analyzed between the groups of patients who received opiates and those who did not.
Results: Of the 125 patient charts reviewed, 90 patients (72%) received opioid analgesics during their hospitalization. The average length of stay for the opioid group was 4.2 days compared to 3.4 days in the non-opioid group (p = 0.146). The mean IV morphine equivalents per day for those who received opioids was 14.74. Celecoxib (23.3% vs 2.8%, p 0.005), gabapentin/pregabalin (40% vs. 20%, p 0.018) and ketorolac (55.5% vs. 2.8%, p < 0.001) use was significantly higher in the opioid cohort.
Discussion: Patients with a prior diagnosis of inflammatory bowel disease who were hospitalized at our hospital in a community setting were associated with a high rate of opioid use. Those who received opioids while hospitalized were more likely to receive other non-opioid analgesics. Consequently, there is ample opportunity to limit opioid use and improve overall outcomes at our institution.
Disclosures:
Andrew Bensinger indicated no relevant financial relationships.
Tess Petersen indicated no relevant financial relationships.
Julianna Tantum indicated no relevant financial relationships.
Adam Kaufman indicated no relevant financial relationships.
Andrew Bensinger, DO, Tess Petersen, MD, Julianna Tantum, DO, Adam Kaufman, MD. E0403 - Opioid Exposure in Hospitalized Patients With Inflammatory Bowel Disease, in a Community Setting, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
