Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0034 - Poorly Cohesive Carcinoma of Gallbladder Presenting as Metastatic Gastric Outlet Obstruction
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Hassan Zreik, MD
Henry Ford Jackson
Dearborn, MI
Presenting Author(s)
Hassan Zreik, MD, Parth M. Patel, MD, Sruthi Ramanan, MD, Zarqa Yasin, MD, Priya Menon, MD, Vrajesh Parmar, MD, Merritt Bern, MD
Henry Ford Jackson, Jackson, MI
Introduction: Gallbladder carcinoma (GBCA) is the most common malignancy of the biliary tract and the fifth most common gastrointestinal malignancy. Gallbladder adenocarcinoma is the most common histological subtype, accounting for about 90-95% of all GBCA. The World Health Organization coined the term ‘poorly cohesive carcinoma’ (PCC) for a subset of GBCA that was previously known as “signet ring cell” or “diffuse infiltrative” type tumors. PCC is an extremely rare subset of GBCA that is highly aggressive.
Case Description/Methods: The patient is a 77-year-old male with a medical history significant for stage 1 lung adenocarcinoma s/p lobectomy and gallbladder carcinoma s/p resection and chemotherapy who presented to the outpatient GI clinic for postprandial pain and abdominal fullness. An upper GI series showed a high-grade gastric outlet obstruction with retained gastric contents and minimal passage of barium. An EGD with biopsy was then completed, which showed a pyloric stricture.
Gastric biopsies revealed metastatic poorly cohesive carcinoma of gallbladder origin. The patient underwent an EGD with the placement of a metal duodenal stent to relieve the metastatic gastric outlet obstruction.
Discussion: Although gallbladder carcinoma is a common GI malignancy, the PCC subtype of GBCA is a rare entity. It accounts for less than 5% of all GBCAs. PCC are aggressive tumors with a median survival of 4 months. PCC type of GBCA has been associated with metastasis to various locations including meninges, skin, bone and pulmonary vasculature. However, gastric outlet obstruction secondary to the PCC is yet to be reported. Histopathologically, PCCs from the gallbladder have classically demonstrated sheets of signet ring cells, which were not present in our case.
Untreated chronic symptomatic cholelithiasis plays a major role in developing GBCA. Pathological examination of our patient’s gallbladder specimen showed evidence of chronic cholecystitis with cholelithiasis. Given the rarity, the pathogenesis behind the development of PCC is unclear. One of the proposed mechanisms involves the presence of pluripotent cells that can differentiate into different types of metaplastic cells leading to metaplasia-dysplasia-carcinoma pathway. Due to the aggressive nature of this tumor, traditional treatments including cholecystectomy have failed to improve the outcome. This warrants further large-scale studies to evaluate the pathogenesis and treatment options for PCC.
Disclosures:
Hassan Zreik, MD, Parth M. Patel, MD, Sruthi Ramanan, MD, Zarqa Yasin, MD, Priya Menon, MD, Vrajesh Parmar, MD, Merritt Bern, MD. A0034 - Poorly Cohesive Carcinoma of Gallbladder Presenting as Metastatic Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Henry Ford Jackson, Jackson, MI
Introduction: Gallbladder carcinoma (GBCA) is the most common malignancy of the biliary tract and the fifth most common gastrointestinal malignancy. Gallbladder adenocarcinoma is the most common histological subtype, accounting for about 90-95% of all GBCA. The World Health Organization coined the term ‘poorly cohesive carcinoma’ (PCC) for a subset of GBCA that was previously known as “signet ring cell” or “diffuse infiltrative” type tumors. PCC is an extremely rare subset of GBCA that is highly aggressive.
Case Description/Methods: The patient is a 77-year-old male with a medical history significant for stage 1 lung adenocarcinoma s/p lobectomy and gallbladder carcinoma s/p resection and chemotherapy who presented to the outpatient GI clinic for postprandial pain and abdominal fullness. An upper GI series showed a high-grade gastric outlet obstruction with retained gastric contents and minimal passage of barium. An EGD with biopsy was then completed, which showed a pyloric stricture.
Gastric biopsies revealed metastatic poorly cohesive carcinoma of gallbladder origin. The patient underwent an EGD with the placement of a metal duodenal stent to relieve the metastatic gastric outlet obstruction.
Discussion: Although gallbladder carcinoma is a common GI malignancy, the PCC subtype of GBCA is a rare entity. It accounts for less than 5% of all GBCAs. PCC are aggressive tumors with a median survival of 4 months. PCC type of GBCA has been associated with metastasis to various locations including meninges, skin, bone and pulmonary vasculature. However, gastric outlet obstruction secondary to the PCC is yet to be reported. Histopathologically, PCCs from the gallbladder have classically demonstrated sheets of signet ring cells, which were not present in our case.
Untreated chronic symptomatic cholelithiasis plays a major role in developing GBCA. Pathological examination of our patient’s gallbladder specimen showed evidence of chronic cholecystitis with cholelithiasis. Given the rarity, the pathogenesis behind the development of PCC is unclear. One of the proposed mechanisms involves the presence of pluripotent cells that can differentiate into different types of metaplastic cells leading to metaplasia-dysplasia-carcinoma pathway. Due to the aggressive nature of this tumor, traditional treatments including cholecystectomy have failed to improve the outcome. This warrants further large-scale studies to evaluate the pathogenesis and treatment options for PCC.
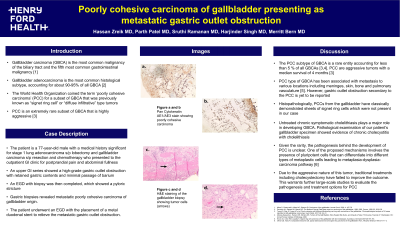
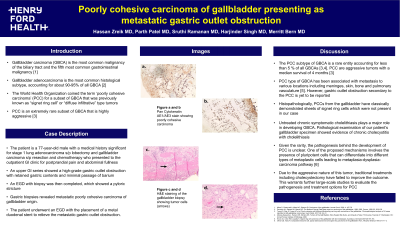
Figure: Figure 1: a. & b. Pan Cytokeratin AE1/AE3 stain showing poorly cohesive carcinoma c. & d. H&E staining of the gallbladder biopsy showing tumor cells (arrows)
Disclosures:
Hassan Zreik indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Sruthi Ramanan indicated no relevant financial relationships.
Zarqa Yasin indicated no relevant financial relationships.
Priya Menon indicated no relevant financial relationships.
Vrajesh Parmar indicated no relevant financial relationships.
Merritt Bern indicated no relevant financial relationships.
Hassan Zreik, MD, Parth M. Patel, MD, Sruthi Ramanan, MD, Zarqa Yasin, MD, Priya Menon, MD, Vrajesh Parmar, MD, Merritt Bern, MD. A0034 - Poorly Cohesive Carcinoma of Gallbladder Presenting as Metastatic Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
