Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0476 - Case of a Severe Cholecystocutaneous Fistula
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Charlotte H. Campbell, MD
Atrium Health Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Charlotte H. Campbell, MD, Swati Pawa, MD
Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Cholecystocutaneous fistulae (aberrant communications of the gallbladder with the skin) have been recognized since the 17th century as possible complications of neglected gallbladder disease. However, in the era of modern medicine they remain uncommon.
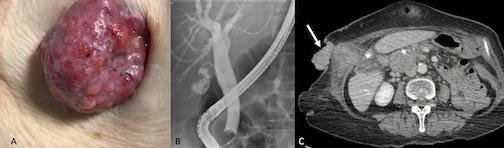
Case Description/Methods: An 83 year-old female with a history of anxiety, depression, and a self-inflicted abdominal gunshot wound presented to our institution 2 years ago with acute calculous cholecystitis and choledocholithiasis. She declined surgery and endoscopic management and was treated with percutaneous cholecystostomy drainage and antibiotics. Subsequent clinical course included multiple tube changes with complaints of recurrent drain dislodgement, leakage, and weight loss. Her cholecystostomy was changed to a percutaneous transhepatic biliary drain. She ultimately presented to the gastroenterology clinic for internalization of her biliary drain. On examination, a large palpable mass was seen in the right upper quadrant with serosanguinous and bloody drainage, consistent with chronic gallbladder extrusion from the abdominal wall. ERCP with removal of percutaneous drain, sphincterotomy, stone extraction, and stent placement was performed. CT abdomen showed a gallbladder mass extending into hepatic segment V as well as through the right abdominal musculature to the skin surface. Enlarged retroperitoneal adenopathy was concerning for metastatic involvement. The patient was deemed a poor surgical candidate, and she opted for hospice care.
Discussion: Cholecystocutaneous fistula is a recognized sequela of unresolved gallbladder inflammation, usually due to persistent biliary outflow obstruction. Other causes may include trauma, iatrogenic causes, gallbladder perforation, or carcinomas. Fistulae may also develop along the track of percutaneous drains following cholecystostomy for management of acute cholecystitis. Surgical management of cholecystocutaneous fistulae with either laparoscopic or open cholecystectomies and fistulae resections have been described with good success. Cholecystocutaneous fistulae in the setting of gallbladder malignancy have poor outcomes due to the spread to adjacent structures. Improved imaging diagnosis of gallstone and gallbladder disease, antibiotic therapies, early surgical intervention for gallbladder disease, and endoscopic alleviation of biliary outflow obstructions have made such a presentation of cholecystocutaneous fistula a rarely seen phenomenon.
Disclosures:
Charlotte H. Campbell, MD, Swati Pawa, MD. B0476 - Case of a Severe Cholecystocutaneous Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Cholecystocutaneous fistulae (aberrant communications of the gallbladder with the skin) have been recognized since the 17th century as possible complications of neglected gallbladder disease. However, in the era of modern medicine they remain uncommon.
Case Description/Methods: An 83 year-old female with a history of anxiety, depression, and a self-inflicted abdominal gunshot wound presented to our institution 2 years ago with acute calculous cholecystitis and choledocholithiasis. She declined surgery and endoscopic management and was treated with percutaneous cholecystostomy drainage and antibiotics. Subsequent clinical course included multiple tube changes with complaints of recurrent drain dislodgement, leakage, and weight loss. Her cholecystostomy was changed to a percutaneous transhepatic biliary drain. She ultimately presented to the gastroenterology clinic for internalization of her biliary drain. On examination, a large palpable mass was seen in the right upper quadrant with serosanguinous and bloody drainage, consistent with chronic gallbladder extrusion from the abdominal wall. ERCP with removal of percutaneous drain, sphincterotomy, stone extraction, and stent placement was performed. CT abdomen showed a gallbladder mass extending into hepatic segment V as well as through the right abdominal musculature to the skin surface. Enlarged retroperitoneal adenopathy was concerning for metastatic involvement. The patient was deemed a poor surgical candidate, and she opted for hospice care.
Discussion: Cholecystocutaneous fistula is a recognized sequela of unresolved gallbladder inflammation, usually due to persistent biliary outflow obstruction. Other causes may include trauma, iatrogenic causes, gallbladder perforation, or carcinomas. Fistulae may also develop along the track of percutaneous drains following cholecystostomy for management of acute cholecystitis. Surgical management of cholecystocutaneous fistulae with either laparoscopic or open cholecystectomies and fistulae resections have been described with good success. Cholecystocutaneous fistulae in the setting of gallbladder malignancy have poor outcomes due to the spread to adjacent structures. Improved imaging diagnosis of gallstone and gallbladder disease, antibiotic therapies, early surgical intervention for gallbladder disease, and endoscopic alleviation of biliary outflow obstructions have made such a presentation of cholecystocutaneous fistula a rarely seen phenomenon.
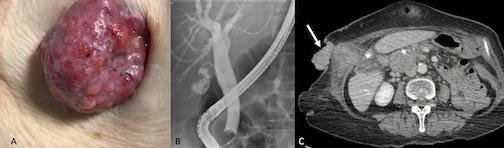
Figure: A patient found to have cholecystocutaneous fistula with (A) gallbladder extruding from the abdominal wall, (B) occlusion cholangiogram post- removal of multiple common bile duct stones showing dilated CBD and cholelithiasis in an irregular, contracted gallbladder, and (C) CT scan showing a mass (star) with extrusion of gallbladder through the liver and skin (arrow).
Disclosures:
Charlotte Campbell indicated no relevant financial relationships.
Swati Pawa indicated no relevant financial relationships.
Charlotte H. Campbell, MD, Swati Pawa, MD. B0476 - Case of a Severe Cholecystocutaneous Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
