Back

Poster Session E - Tuesday Afternoon
Category: Interventional Endoscopy
E0443 - When One Stent Fails, Another One to the Rescue: A Novel Approach to Managing Small Post-Op Gastric Leaks Following Laparoscopic Sleeve Gastrectomy
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Reginald Lafleur, MD
Wyckoff Heights Medical Center
Brooklyn, NY
Presenting Author(s)
Reginald Lafleur, MD1, Joseph Dayrit, BSc2, Susan Ramdhaney, MD3, Leaque Ahmed, MD1, Shazhad Iqbal, MD, FACG1
1Wyckoff Heights Medical Center, Brooklyn, NY; 2St. George's University School of Medicine, Brooklyn, NY; 3Wyckoff Heights Medical Center/ St. George's University School of Medicine, Brooklyn, NY
Introduction: Laparoscopic sleeve gastrectomy (LSG) is a commonly used procedure in the surgical management of Obesity. However, post-op complications such as gastric leaks and their sequelae pose challenges. We present a case of a novel alternative in managing a small contained post-op gastric leak, which was difficult to define radiographically but was visible endoscopically causing the patient symptoms.
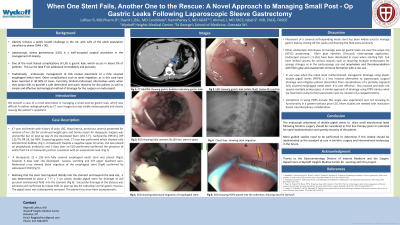
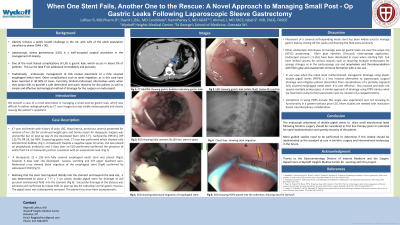
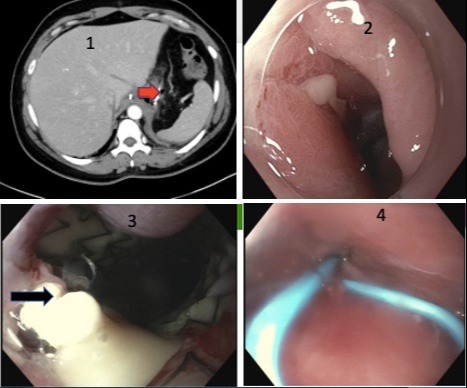
Case Description/Methods: A 47 year old female with history of prior LSG, hiatal hernia, pernicious anemia presented for revision of her LSG for continued weight gain and hernia repair for dyspepsia. Surgery was uneventful but on post-op day 25 she developed fever (101.5 F), tachycardia (HR125), BP 131/74, RR 18, Sat 96%. Suspecting gastric leak, CT scan was performed which showed only extraluminal bubbles (Fig 1). Despite a negative upper GI series she was placed on prophylactic antibiotics and 3 days later an EGD performed confirmed the presence of pus 3-4 cm below GE junction consistent with an anastomotic leak. (Fig 2) . A therapeutic 23 x 150 mm fully covered esophageal metal stent was placed , however 6 days later she developed nausea, vomiting and left upper quadrant pain. Abdominal x-ray showed distal migration of the esophageal stent confirmed by subsequent EGD (Fig3). At that point, the stent was removed and a 7 Fr x 7 cm plastic double pigtail stent was placed into the abscess cavity for drainage of purulent fluid (Fig 4) into the stomach. Successful drainage of the abscess was achieved and confirmed by repeat EGD on post-op day 83 indicating normal gastric mucosa. The pigtail stent was subsequently removed. The patient has since been asymptomatic.
Discussion: Endoscopic stenting has been widely used to manage post-op LSG gastric leak by closing off the cavity and draining extra-luminally. However, its migration causes significant patient discomfort, allows persistent fluid collection and abscess formation, delays healing and prolongs hospital stay. We propose a novel technique of mimicking a transgastric pseudocyst drain using a double pigtail plastic stent as an effective method of treating a small post-op LSG gastric leak after esophageal stent migration. In our patient, this technique hastened recovery, and decreased morbidity- related outcomes and hence this technique can be considered as future first line treatment.
Disclosures:
Reginald Lafleur, MD1, Joseph Dayrit, BSc2, Susan Ramdhaney, MD3, Leaque Ahmed, MD1, Shazhad Iqbal, MD, FACG1. E0443 - When One Stent Fails, Another One to the Rescue: A Novel Approach to Managing Small Post-Op Gastric Leaks Following Laparoscopic Sleeve Gastrectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wyckoff Heights Medical Center, Brooklyn, NY; 2St. George's University School of Medicine, Brooklyn, NY; 3Wyckoff Heights Medical Center/ St. George's University School of Medicine, Brooklyn, NY
Introduction: Laparoscopic sleeve gastrectomy (LSG) is a commonly used procedure in the surgical management of Obesity. However, post-op complications such as gastric leaks and their sequelae pose challenges. We present a case of a novel alternative in managing a small contained post-op gastric leak, which was difficult to define radiographically but was visible endoscopically causing the patient symptoms.
Case Description/Methods: A 47 year old female with history of prior LSG, hiatal hernia, pernicious anemia presented for revision of her LSG for continued weight gain and hernia repair for dyspepsia. Surgery was uneventful but on post-op day 25 she developed fever (101.5 F), tachycardia (HR125), BP 131/74, RR 18, Sat 96%. Suspecting gastric leak, CT scan was performed which showed only extraluminal bubbles (Fig 1). Despite a negative upper GI series she was placed on prophylactic antibiotics and 3 days later an EGD performed confirmed the presence of pus 3-4 cm below GE junction consistent with an anastomotic leak. (Fig 2) . A therapeutic 23 x 150 mm fully covered esophageal metal stent was placed , however 6 days later she developed nausea, vomiting and left upper quadrant pain. Abdominal x-ray showed distal migration of the esophageal stent confirmed by subsequent EGD (Fig3). At that point, the stent was removed and a 7 Fr x 7 cm plastic double pigtail stent was placed into the abscess cavity for drainage of purulent fluid (Fig 4) into the stomach. Successful drainage of the abscess was achieved and confirmed by repeat EGD on post-op day 83 indicating normal gastric mucosa. The pigtail stent was subsequently removed. The patient has since been asymptomatic.
Discussion: Endoscopic stenting has been widely used to manage post-op LSG gastric leak by closing off the cavity and draining extra-luminally. However, its migration causes significant patient discomfort, allows persistent fluid collection and abscess formation, delays healing and prolongs hospital stay. We propose a novel technique of mimicking a transgastric pseudocyst drain using a double pigtail plastic stent as an effective method of treating a small post-op LSG gastric leak after esophageal stent migration. In our patient, this technique hastened recovery, and decreased morbidity- related outcomes and hence this technique can be considered as future first line treatment.
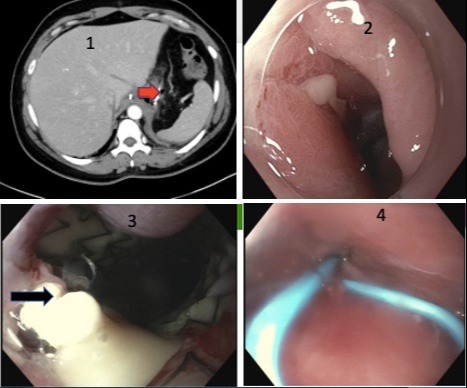
Figure: Figure
(1) CT Ab/Pelvis arrowhead notes extraluminal bubbles near the GE Junction (arrowhead)
(2) EGD showing white fluid (pus) 3 – 4 cms below the EG junction consistent with post-op LSG gastric leak
(3) EGD showing increased pus anterior to tip of migrated stent (arrowhead)
(4) Placement of double pigtail for successful drainage of purulent material
(1) CT Ab/Pelvis arrowhead notes extraluminal bubbles near the GE Junction (arrowhead)
(2) EGD showing white fluid (pus) 3 – 4 cms below the EG junction consistent with post-op LSG gastric leak
(3) EGD showing increased pus anterior to tip of migrated stent (arrowhead)
(4) Placement of double pigtail for successful drainage of purulent material
Disclosures:
Reginald Lafleur indicated no relevant financial relationships.
Joseph Dayrit indicated no relevant financial relationships.
Susan Ramdhaney indicated no relevant financial relationships.
Leaque Ahmed indicated no relevant financial relationships.
Shazhad Iqbal indicated no relevant financial relationships.
Reginald Lafleur, MD1, Joseph Dayrit, BSc2, Susan Ramdhaney, MD3, Leaque Ahmed, MD1, Shazhad Iqbal, MD, FACG1. E0443 - When One Stent Fails, Another One to the Rescue: A Novel Approach to Managing Small Post-Op Gastric Leaks Following Laparoscopic Sleeve Gastrectomy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
