Back
Poster Session A - Sunday Afternoon
Category: Esophagus
A0215 - Gurvit Syndrome: An Unusual Presentation of Upper Gastrointestinal Hemorrhage in a Case of Hypovolemic Shock
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
- FA
Farhan Ali, DO
Arnot Ogden Medical Center
Ijamsville, MD
Presenting Author(s)
Farhan Ali, DO1, Gary Valvano, DO2, Zohaib Ahmad, BS3, Harsha Surath, MD2, Siri Chadalavada, MD2
1Arnot Ogden Medical Center, Ijamsville, MD; 2Arnot Ogden Medical Center, Elmira, NY; 3LECOM, Plainview, NY
Introduction: Acute Esophageal Necrosis (AEN) is a rare disorder with a high associated mortality often seen in the setting of ischemia is considered the most plausible etiology. Other associated conditions include coronary artery disease, gastric outlet obstruction, infection, trauma, and alcohol ingestion. Diagnosis is made endoscopically, and findings are typically characterized as circumferential, macerated mucosa appearing black. We present a case of a 69-year-old female who was admitted for diabetic ketoacidosis, who ultimately developed acute hypoxemic respiratory failure and upper gastrointestinal hemorrhage, and was found on upper endoscopy, to have distal esophageal necrosis.
Case Description/Methods: A 69 y/o female with a past medical history notable for poorly controlled type 2 diabetes mellitus, pulmonary hypertension, systolic heart failure (EF 40-45%) presented to the emergency room with complaints of intractable nausea and vomiting.
Upon initial lab workup, she was noted to have a hemoglobin of 17.3, MCV 101, WBC 37.9, Platelets 275K, sodium 138, potassium 6.5, chloride 103, bicarbonate 17, glucose 241, BUN 97, creatinine 2.3, albumin 2.3, total bilirubin 0.4, alkaline phosphatase 73, AST 2985, ALT 1945, LDH 8074. PT 26.1, INR 2.3, lactic acid 10.3.
She was sent to the ICU and managed for DKA with anion gap of 25 on arrival with concomitant hypoxemic respiratory failure. Within 24 hours the patient became hypotensive requiring maximal pressor support and was eventually intubated. Two hours later she was noted to have 1200 mL of dark black material suctioned from her NG tube, and was noted to be passing melenic stool. Repeat hemoglobin was noted to be 5.4g/dL.
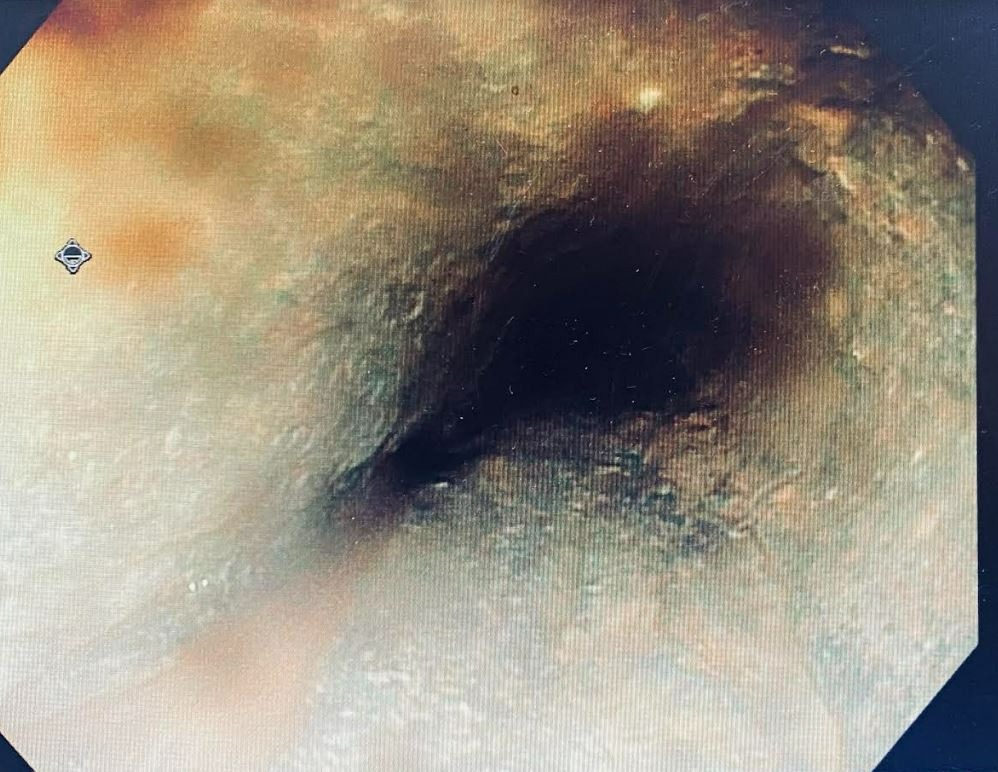
An EGD was performed, which showed a necrotic appearing esophagus involving the distal 2/3 of the esophagus (Figure 1). A distorted pyloric channel with large ulceration encompassing the entire duodenal bulb. The patient was continued on maximal pressor support but despite medical intervention, she ultimately expired 6 hours later.
Discussion: Patients with AEN often have hemodynamic compromise resulting in ischemia. Esophageal arterial supply differs based on region. The proximal and mid esophagus are supplied from inferior thyroid artery, and bronchial aa. The distal esophagus is supplied by the left gastric artery and has a relatively poor collateral supply. Management involves adequate hemodynamic support, intravenous acid suppression. Unfortunately, overall mortality of AEN remains high, estimated to be 32%.
Disclosures:
Farhan Ali, DO1, Gary Valvano, DO2, Zohaib Ahmad, BS3, Harsha Surath, MD2, Siri Chadalavada, MD2. A0215 - Gurvit Syndrome: An Unusual Presentation of Upper Gastrointestinal Hemorrhage in a Case of Hypovolemic Shock, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Arnot Ogden Medical Center, Ijamsville, MD; 2Arnot Ogden Medical Center, Elmira, NY; 3LECOM, Plainview, NY
Introduction: Acute Esophageal Necrosis (AEN) is a rare disorder with a high associated mortality often seen in the setting of ischemia is considered the most plausible etiology. Other associated conditions include coronary artery disease, gastric outlet obstruction, infection, trauma, and alcohol ingestion. Diagnosis is made endoscopically, and findings are typically characterized as circumferential, macerated mucosa appearing black. We present a case of a 69-year-old female who was admitted for diabetic ketoacidosis, who ultimately developed acute hypoxemic respiratory failure and upper gastrointestinal hemorrhage, and was found on upper endoscopy, to have distal esophageal necrosis.
Case Description/Methods: A 69 y/o female with a past medical history notable for poorly controlled type 2 diabetes mellitus, pulmonary hypertension, systolic heart failure (EF 40-45%) presented to the emergency room with complaints of intractable nausea and vomiting.
Upon initial lab workup, she was noted to have a hemoglobin of 17.3, MCV 101, WBC 37.9, Platelets 275K, sodium 138, potassium 6.5, chloride 103, bicarbonate 17, glucose 241, BUN 97, creatinine 2.3, albumin 2.3, total bilirubin 0.4, alkaline phosphatase 73, AST 2985, ALT 1945, LDH 8074. PT 26.1, INR 2.3, lactic acid 10.3.
She was sent to the ICU and managed for DKA with anion gap of 25 on arrival with concomitant hypoxemic respiratory failure. Within 24 hours the patient became hypotensive requiring maximal pressor support and was eventually intubated. Two hours later she was noted to have 1200 mL of dark black material suctioned from her NG tube, and was noted to be passing melenic stool. Repeat hemoglobin was noted to be 5.4g/dL.
An EGD was performed, which showed a necrotic appearing esophagus involving the distal 2/3 of the esophagus (Figure 1). A distorted pyloric channel with large ulceration encompassing the entire duodenal bulb. The patient was continued on maximal pressor support but despite medical intervention, she ultimately expired 6 hours later.
Discussion: Patients with AEN often have hemodynamic compromise resulting in ischemia. Esophageal arterial supply differs based on region. The proximal and mid esophagus are supplied from inferior thyroid artery, and bronchial aa. The distal esophagus is supplied by the left gastric artery and has a relatively poor collateral supply. Management involves adequate hemodynamic support, intravenous acid suppression. Unfortunately, overall mortality of AEN remains high, estimated to be 32%.
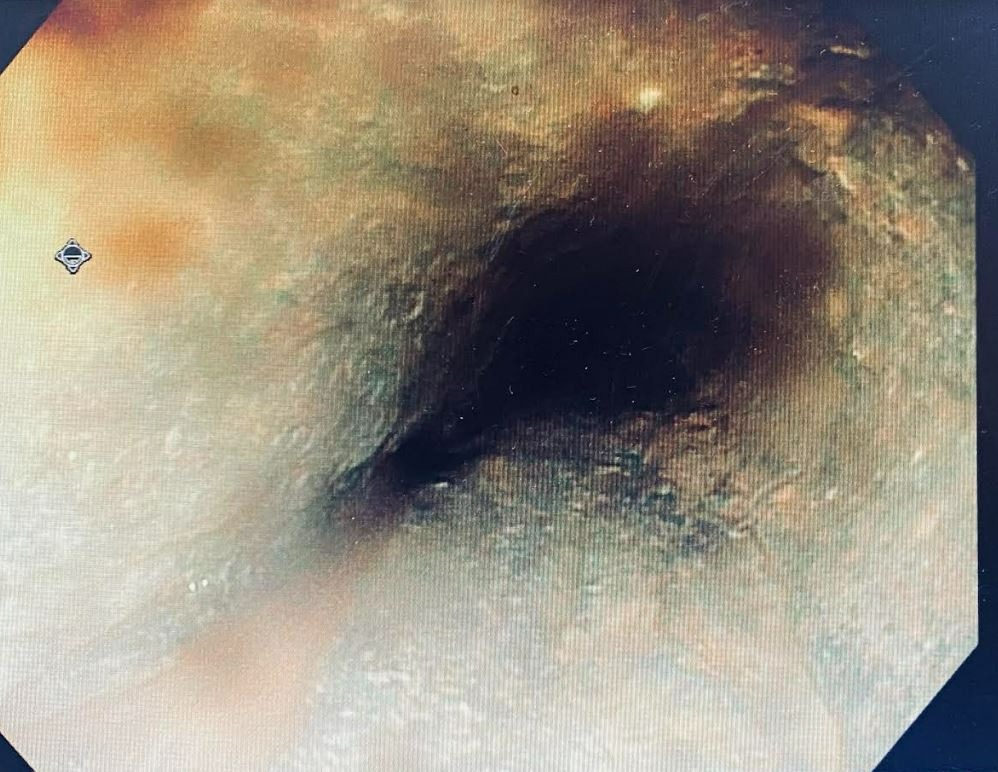
Figure: necrotic appearing distal esophagus
Disclosures:
Farhan Ali indicated no relevant financial relationships.
Gary Valvano indicated no relevant financial relationships.
Zohaib Ahmad indicated no relevant financial relationships.
Harsha Surath indicated no relevant financial relationships.
Siri Chadalavada indicated no relevant financial relationships.
Farhan Ali, DO1, Gary Valvano, DO2, Zohaib Ahmad, BS3, Harsha Surath, MD2, Siri Chadalavada, MD2. A0215 - Gurvit Syndrome: An Unusual Presentation of Upper Gastrointestinal Hemorrhage in a Case of Hypovolemic Shock, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
