Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0266 - Dysphagia, Rings and Furrows, Oh My! A Rare Cause of Benign Esophageal Stenosis
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

- AT
Abirami Thiyagarajan, MD
Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Abirami Thiyagarajan, MD, Subhankar Chakraborty, MD, PhD
Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Lichen planus is a chronic, inflammatory autoimmune disease found in 0.5-2.0% of the population (predominantly females age 44 to 79) that can affect the skin, nails and mucosal membranes. Lichen planus is a rare cause of esophagitis and esophageal stricture and stenosis.
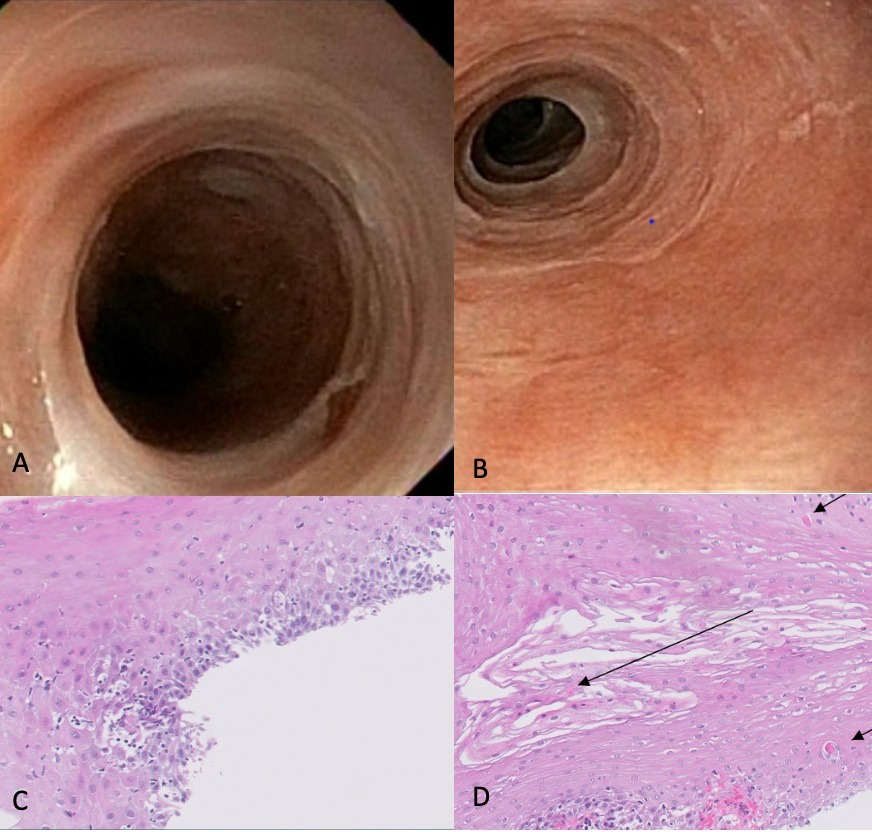
Case Description/Methods: A 52 year old female with a history of reflux presented with progressive dysphagia to solids for 18 months with slow transit, odynophagia and pills getting stuck. She had a 20 pound weight loss over the last 3-4 months. She also had reflux symptoms with regurgitation of food. EGD at outside hospital reportedly showed esophageal stenosis requiring dilation and biopsies of esophagus. She was previously on a proton pump inhibitor but now unable to swallow pills. Physical exam was unremarkable with no rashes or oral lesions. Stenosis in the lower esophagus < 1cm in length was found on EGD with mucosal changes suspicious for eosinophilic esophagitis (EoE). Pathology showed lymphocytes and eosinophils not meeting criteria for EoE. Repeat EGD off of lansoprazole demonstrated benign stenosis in the distal esophagus that was dilated and mucosal changes suspicious for EoE. Biopsies demonstrated basilar lymphocytosis and apoptotic keratinocytes concerning for lichenoid esophagitis. She underwent multiple endoscopic dilations for recurrent, benign esophageal stenosis eventually complicated by deep mucosal tear requiring esophageal stenting. Stent was removed and she was started on swallowed budesonide to treat lichen planus of the esophagus. During repeat EGD, she underwent endoscopic, intralesional triamcinolone injections with 5mg injected into esophageal stricture.
Discussion: Esophageal involvement in lichen planus is rare and can occur without dermatologic or oral involvement. Endoscopic findings include mucosal sloughing and tearing; pseudomembranes; hyperkeratosis; trachealization; and stenosis/stricture. Microscopic findings include band-like lichenoid lymphocytic infiltrate involving the superficial lamina propria and basal epithelium and eosinophilic apoptotic keratinocytes (Civatte bodies) in the basal layer. While there are not clear guidelines on diagnostic criteria or management of esophageal lichen planus, treatment includes topical and systemic corticosteroids. Endoscopic dilation is the mainstay of treatment for esophageal strictures and stenosis. Intralesional, endoscopic steroid injection is an option for recurrent, benign esophageal stenosis that can increase the interval between dilations.
Disclosures:
Abirami Thiyagarajan, MD, Subhankar Chakraborty, MD, PhD. C0266 - Dysphagia, Rings and Furrows, Oh My! A Rare Cause of Benign Esophageal Stenosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Lichen planus is a chronic, inflammatory autoimmune disease found in 0.5-2.0% of the population (predominantly females age 44 to 79) that can affect the skin, nails and mucosal membranes. Lichen planus is a rare cause of esophagitis and esophageal stricture and stenosis.
Case Description/Methods: A 52 year old female with a history of reflux presented with progressive dysphagia to solids for 18 months with slow transit, odynophagia and pills getting stuck. She had a 20 pound weight loss over the last 3-4 months. She also had reflux symptoms with regurgitation of food. EGD at outside hospital reportedly showed esophageal stenosis requiring dilation and biopsies of esophagus. She was previously on a proton pump inhibitor but now unable to swallow pills. Physical exam was unremarkable with no rashes or oral lesions. Stenosis in the lower esophagus < 1cm in length was found on EGD with mucosal changes suspicious for eosinophilic esophagitis (EoE). Pathology showed lymphocytes and eosinophils not meeting criteria for EoE. Repeat EGD off of lansoprazole demonstrated benign stenosis in the distal esophagus that was dilated and mucosal changes suspicious for EoE. Biopsies demonstrated basilar lymphocytosis and apoptotic keratinocytes concerning for lichenoid esophagitis. She underwent multiple endoscopic dilations for recurrent, benign esophageal stenosis eventually complicated by deep mucosal tear requiring esophageal stenting. Stent was removed and she was started on swallowed budesonide to treat lichen planus of the esophagus. During repeat EGD, she underwent endoscopic, intralesional triamcinolone injections with 5mg injected into esophageal stricture.
Discussion: Esophageal involvement in lichen planus is rare and can occur without dermatologic or oral involvement. Endoscopic findings include mucosal sloughing and tearing; pseudomembranes; hyperkeratosis; trachealization; and stenosis/stricture. Microscopic findings include band-like lichenoid lymphocytic infiltrate involving the superficial lamina propria and basal epithelium and eosinophilic apoptotic keratinocytes (Civatte bodies) in the basal layer. While there are not clear guidelines on diagnostic criteria or management of esophageal lichen planus, treatment includes topical and systemic corticosteroids. Endoscopic dilation is the mainstay of treatment for esophageal strictures and stenosis. Intralesional, endoscopic steroid injection is an option for recurrent, benign esophageal stenosis that can increase the interval between dilations.
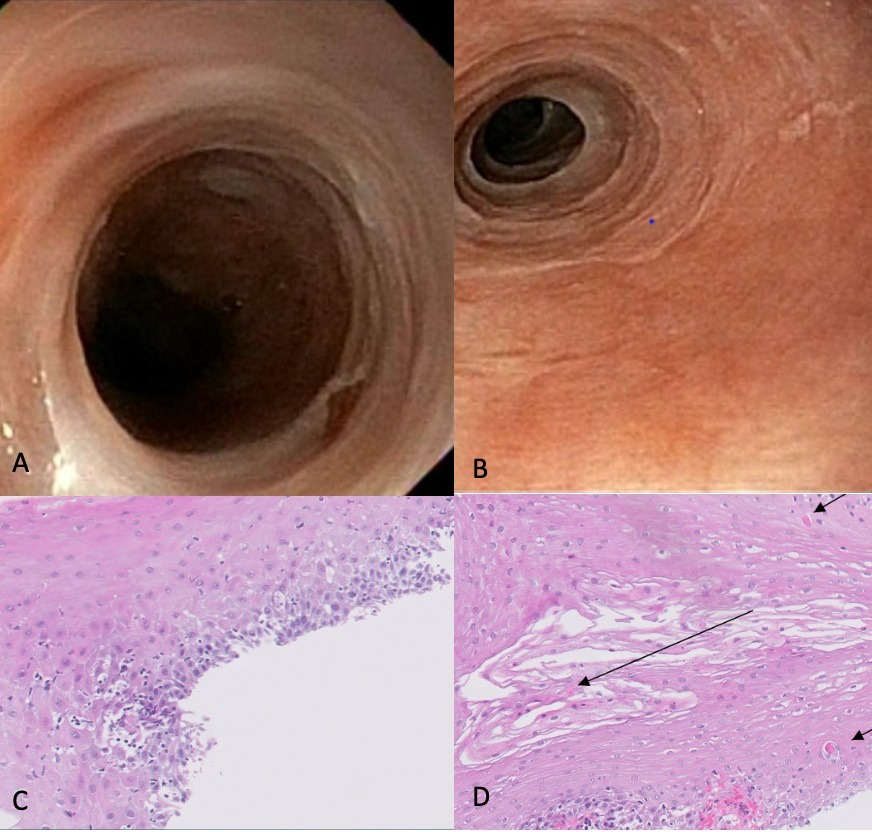
Figure: A. Mucosal rings, keratinization and sloughing of esophageal mucosa seen on endoscopically. B. Esophageal stenosis seen endoscopically. C. Esophageal biopsy pathology-basilar lymphocytosis and basal cell hyperplasia. D. Esophageal biopsy pathology- necrotic, esosinophilic keratinocytes (Civatte bodies).
Disclosures:
Abirami Thiyagarajan indicated no relevant financial relationships.
Subhankar Chakraborty indicated no relevant financial relationships.
Abirami Thiyagarajan, MD, Subhankar Chakraborty, MD, PhD. C0266 - Dysphagia, Rings and Furrows, Oh My! A Rare Cause of Benign Esophageal Stenosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

