Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0245 - Holey Esophagus: An Indeterminate Case of a Fenestrated Esophagitis in an Immunocompromised Host
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Dean Rizzi, MD
New York Presbyterian Brooklyn Methodist
Brooklyn, NY
Presenting Author(s)
Dean Rizzi, MD1, Harsh Patel, MD, MPH2, John Patresan, MD3, Michael Castillo, MD3, Daniel Golpanian, MD3, Franklin Kasmin, MD3
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 2NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Immunocompromised patients have increased risk of developing ulcerative esophagitis. The most common etiologies of ulcers are radiation induced, chemotherapy, and opportunistic infections. HSV esophagitis has yellow exudate and discrete, coalescent ulcers, while CMV esophagitis typically has large, shallow, solitary or multiple ulcers located in the mid to distal esophagus. Chemotherapy with radiation therapy and concurrent Gemcitabine and Cisplatin has been reported in up to 52% of severe esophagitis. We present a case of idiopathic esophagitis with a unique endoscopic appearance of multiple fenestrations throughout the esophagus.
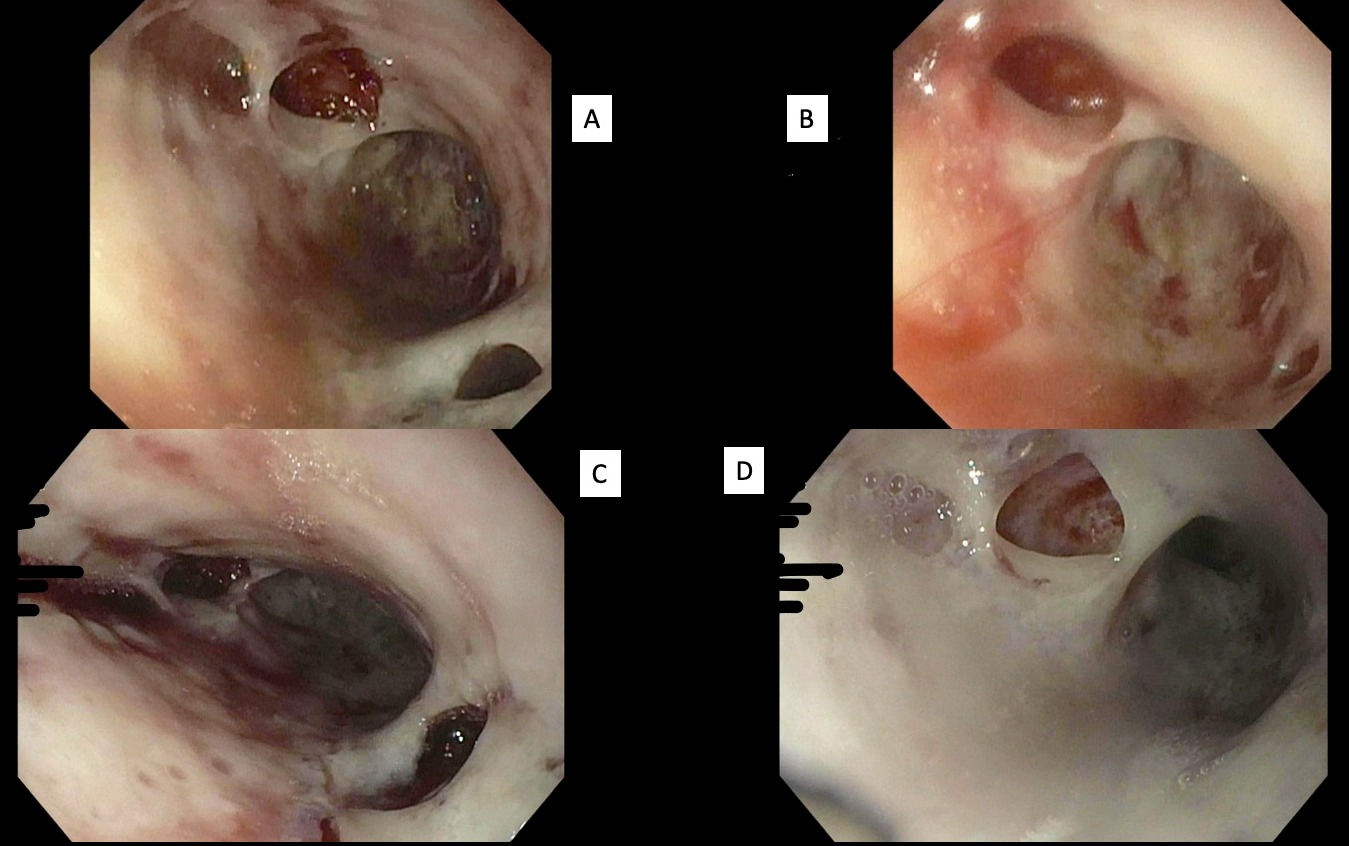
Case Description/Methods: A 66 year old female with past medical history significant for stage 1A Uterine Serous Carcinoma presented to the ED with two days of hematemesis. She reports multiple episodes of emesis with each one subsequently becoming increasingly more bloody. She had received her 5th cycle of Cisplatin and Gemcitabine two days prior to presentation. She underwent an esophagogastroduodenoscopy (EGD) with unique findings of severe inflammation with exudative plaques with fenestrated appearance and oozing of blood. There was initial concern for esophageal perforations, diverticulosis and fistulas however these did not match the clinical presentation. Biopsies were consistent with active esophagitis with necroinflammatory debris consistent with ulcer. Gastrografin esophagram showed no evidence of contrast extravasation ruling out fistulous connections. Stains for CMV and HSV were inconclusive despite adequate tissue sampling.
Discussion: Given the gross appearance of the esophagus on EGD and lack of CMV immunohistochemical conclusivity, the etiology of ulceration in this case is unclear. The most common endoscopic findings of CMV esophagitis are mucosal ulcerations typically located in the mid to distal esophagus. Diagnosis is made by immunohistochemical visualization of cytomegalovirus inclusion bodies within the biopsied tissue. Patients who receive chemotherapy may experience post-infusion related mucositis in addition to immunosuppression. Mucositis occurs via diffuse non-specific chemotherapeutic targeting of tissues with high cell turnover. In our case, the ulceration is focal from the mid to distal portion of the esophagus, more reflective of CMV opposed to the diffuse involvement anticipated in mucositis. We hypothesize that the atypical fenestrated appearance of esophageal mucosa may be a consequence of mucositis with superimposed CMV infection.
Disclosures:
Dean Rizzi, MD1, Harsh Patel, MD, MPH2, John Patresan, MD3, Michael Castillo, MD3, Daniel Golpanian, MD3, Franklin Kasmin, MD3. D0245 - Holey Esophagus: An Indeterminate Case of a Fenestrated Esophagitis in an Immunocompromised Host, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY; 2NewYork Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY; 3New York Presbyterian Brooklyn Methodist Hospital, Brooklyn, NY
Introduction: Immunocompromised patients have increased risk of developing ulcerative esophagitis. The most common etiologies of ulcers are radiation induced, chemotherapy, and opportunistic infections. HSV esophagitis has yellow exudate and discrete, coalescent ulcers, while CMV esophagitis typically has large, shallow, solitary or multiple ulcers located in the mid to distal esophagus. Chemotherapy with radiation therapy and concurrent Gemcitabine and Cisplatin has been reported in up to 52% of severe esophagitis. We present a case of idiopathic esophagitis with a unique endoscopic appearance of multiple fenestrations throughout the esophagus.
Case Description/Methods: A 66 year old female with past medical history significant for stage 1A Uterine Serous Carcinoma presented to the ED with two days of hematemesis. She reports multiple episodes of emesis with each one subsequently becoming increasingly more bloody. She had received her 5th cycle of Cisplatin and Gemcitabine two days prior to presentation. She underwent an esophagogastroduodenoscopy (EGD) with unique findings of severe inflammation with exudative plaques with fenestrated appearance and oozing of blood. There was initial concern for esophageal perforations, diverticulosis and fistulas however these did not match the clinical presentation. Biopsies were consistent with active esophagitis with necroinflammatory debris consistent with ulcer. Gastrografin esophagram showed no evidence of contrast extravasation ruling out fistulous connections. Stains for CMV and HSV were inconclusive despite adequate tissue sampling.
Discussion: Given the gross appearance of the esophagus on EGD and lack of CMV immunohistochemical conclusivity, the etiology of ulceration in this case is unclear. The most common endoscopic findings of CMV esophagitis are mucosal ulcerations typically located in the mid to distal esophagus. Diagnosis is made by immunohistochemical visualization of cytomegalovirus inclusion bodies within the biopsied tissue. Patients who receive chemotherapy may experience post-infusion related mucositis in addition to immunosuppression. Mucositis occurs via diffuse non-specific chemotherapeutic targeting of tissues with high cell turnover. In our case, the ulceration is focal from the mid to distal portion of the esophagus, more reflective of CMV opposed to the diffuse involvement anticipated in mucositis. We hypothesize that the atypical fenestrated appearance of esophageal mucosa may be a consequence of mucositis with superimposed CMV infection.
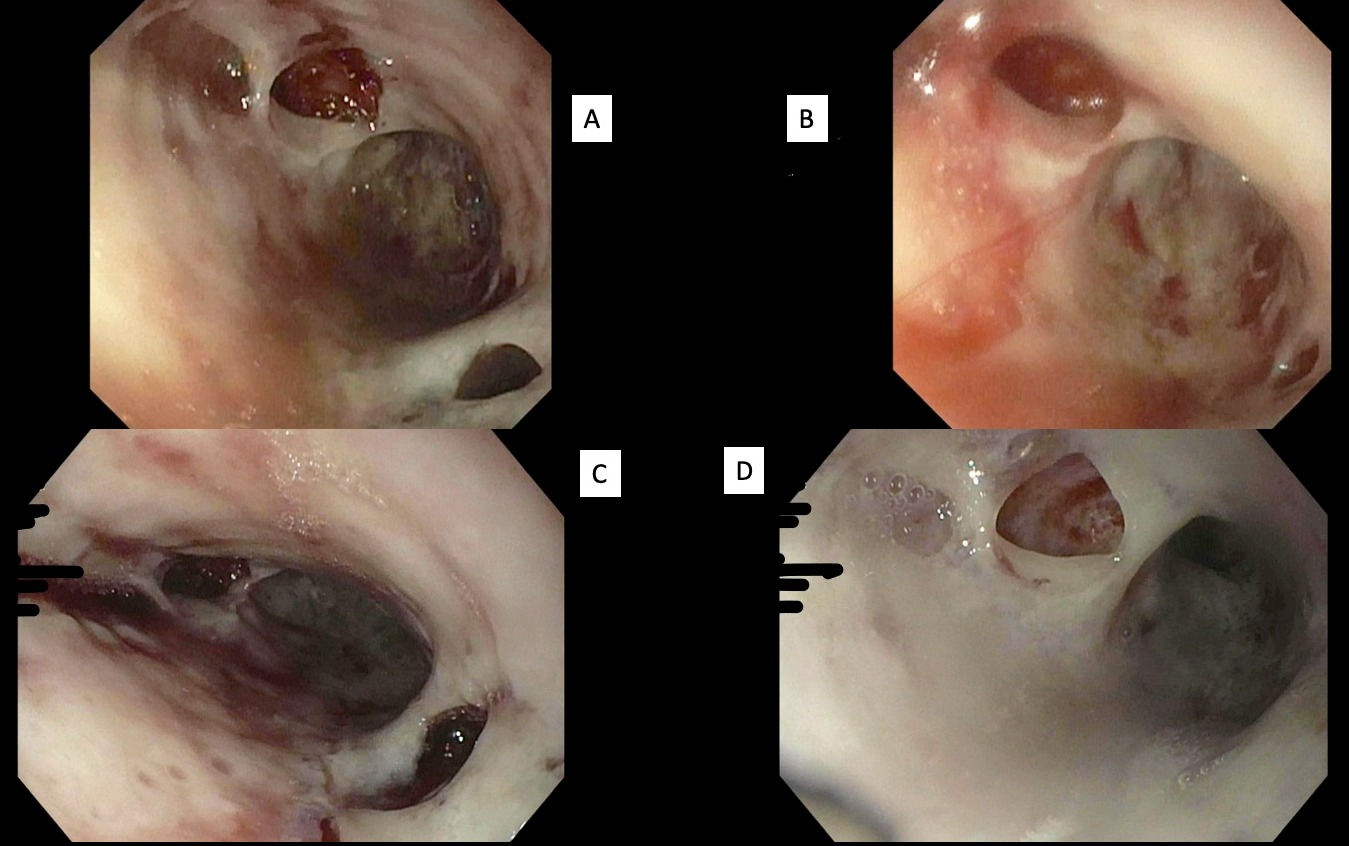
Figure: Image: (A, B, C, D) showing the mid to distal esophagus with multiple shallow ulcers of varying sizes. (C) appears to have oozing of blood and friability. No obvious evidence of fistula, perforation, or diverticulum noted.
Disclosures:
Dean Rizzi indicated no relevant financial relationships.
Harsh Patel indicated no relevant financial relationships.
John Patresan indicated no relevant financial relationships.
Michael Castillo indicated no relevant financial relationships.
Daniel Golpanian indicated no relevant financial relationships.
Franklin Kasmin indicated no relevant financial relationships.
Dean Rizzi, MD1, Harsh Patel, MD, MPH2, John Patresan, MD3, Michael Castillo, MD3, Daniel Golpanian, MD3, Franklin Kasmin, MD3. D0245 - Holey Esophagus: An Indeterminate Case of a Fenestrated Esophagitis in an Immunocompromised Host, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
