Back

Poster Session A - Sunday Afternoon
Category: Biliary/Pancreas
A0068 - Combination of Pancreatic and Hepatic Pseudocyst in a Patient With Pancreatitis: A Case Report
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Brian Sowka, DO
Gundersen Health System
La Crosse, WI
Presenting Author(s)
Brian Sowka, DO, Padmavathi Mali, MD
Gundersen Health System, La Crosse, WI
Introduction: Pancreatic pseudocysts are common occurrences after episodes of acute pancreatitis. Up to 20% of pseudocysts are extra-pancreatic throughout the abdomen including intrahepatic. There are only a few cases of hepatic pseudocysts reported in the literature. We report this unique case with both pancreatic and intrahepatic pseudocysts occurring at the same time in a patient with pancreatitis.
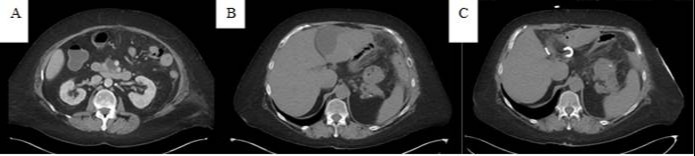
Case Description/Methods: A 56-year-old Caucasian female with history of alcoholism and chronic pancreatitis, presented with epigastric and left upper quadrant abdominal pain radiating to the left shoulder. Examination revealed tenderness in the epigastric and left upper quadrant of the abdomen. Labs showed an elevated lipase of 217 IU/L (13-60), normal total bilirubin and transaminases, hemoglobin of 9.1 g/dL(11.5-15), and slight leukocytosis 12.6 K/uL (3.7-10.4). She was admitted three times in the last 4 months. Prior CT (Computerized Tomography) scan showed pseudocysts in the head and tail of the pancreas. CT scan this admission showed a decreased size of pseudocyst in the pancreatic head from 2.5 cm to 2.2 cm and pancreatic tail from 4.2 cm to 3.7 cm. It also showed two subcapsular fluid collections in the left lobe of the liver measuring 9X5X2cm and 9X7X3 cm. Percutaneous drainage of the hepatic cysts with the placement of a drainage catheter was performed by interventional radiology. 50 mL of bilious appearing fluid was drained with negative gram stain and cultures with an elevated fluid amylase level of 1,765 U/L. The patient’s pain improved and a subsequent CT a few weeks after discharge showed a decrease in the size of the hepatic cysts.
Discussion: This is the first documented case of combined pancreatic and intrahepatic pseudocyst formation. Elevated amylase level in the hepatic fluid analysis confirmed the diagnosis of a hepatic pseudocyst. The interesting fact is that the size of the pancreatic pseudocyst decreased as the hepatic pseudocyst increased because of fluid tracking likely in the pre-renal space or along the hepato-gastric ligament. The diagnosis of hepatic pseudocyst needs to be considered in a patient with new hepatic fluid collection with a recent history of pancreatitis and pancreatic pseudocyst.
Disclosures:
Brian Sowka, DO, Padmavathi Mali, MD. A0068 - Combination of Pancreatic and Hepatic Pseudocyst in a Patient With Pancreatitis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Gundersen Health System, La Crosse, WI
Introduction: Pancreatic pseudocysts are common occurrences after episodes of acute pancreatitis. Up to 20% of pseudocysts are extra-pancreatic throughout the abdomen including intrahepatic. There are only a few cases of hepatic pseudocysts reported in the literature. We report this unique case with both pancreatic and intrahepatic pseudocysts occurring at the same time in a patient with pancreatitis.
Case Description/Methods: A 56-year-old Caucasian female with history of alcoholism and chronic pancreatitis, presented with epigastric and left upper quadrant abdominal pain radiating to the left shoulder. Examination revealed tenderness in the epigastric and left upper quadrant of the abdomen. Labs showed an elevated lipase of 217 IU/L (13-60), normal total bilirubin and transaminases, hemoglobin of 9.1 g/dL(11.5-15), and slight leukocytosis 12.6 K/uL (3.7-10.4). She was admitted three times in the last 4 months. Prior CT (Computerized Tomography) scan showed pseudocysts in the head and tail of the pancreas. CT scan this admission showed a decreased size of pseudocyst in the pancreatic head from 2.5 cm to 2.2 cm and pancreatic tail from 4.2 cm to 3.7 cm. It also showed two subcapsular fluid collections in the left lobe of the liver measuring 9X5X2cm and 9X7X3 cm. Percutaneous drainage of the hepatic cysts with the placement of a drainage catheter was performed by interventional radiology. 50 mL of bilious appearing fluid was drained with negative gram stain and cultures with an elevated fluid amylase level of 1,765 U/L. The patient’s pain improved and a subsequent CT a few weeks after discharge showed a decrease in the size of the hepatic cysts.
Discussion: This is the first documented case of combined pancreatic and intrahepatic pseudocyst formation. Elevated amylase level in the hepatic fluid analysis confirmed the diagnosis of a hepatic pseudocyst. The interesting fact is that the size of the pancreatic pseudocyst decreased as the hepatic pseudocyst increased because of fluid tracking likely in the pre-renal space or along the hepato-gastric ligament. The diagnosis of hepatic pseudocyst needs to be considered in a patient with new hepatic fluid collection with a recent history of pancreatitis and pancreatic pseudocyst.
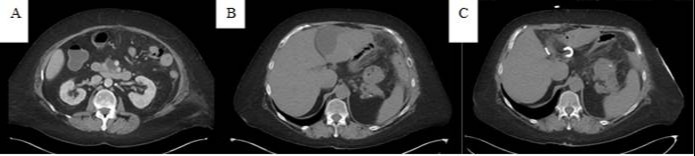
Figure: A – Axial CT showing previous pancreatic pseudocyst prior to admission
B – Axial CT showing new hepatic pseudocyst adjacent to falciform ligament during admission
C – Axial CT showing drain in hepatic pseudocyst
B – Axial CT showing new hepatic pseudocyst adjacent to falciform ligament during admission
C – Axial CT showing drain in hepatic pseudocyst
Disclosures:
Brian Sowka indicated no relevant financial relationships.
Padmavathi Mali indicated no relevant financial relationships.
Brian Sowka, DO, Padmavathi Mali, MD. A0068 - Combination of Pancreatic and Hepatic Pseudocyst in a Patient With Pancreatitis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
