Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0521 - Flood Syndrome: A Herniating Complication of Liver Cirrhosis
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
Prabhat Kumar, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Prabhat Kumar, MD1, Michael M. Cymbal, BS2, Eduard Krishtopaytis, MD1, Somtochukwu Onwuzo, MD1, Antoine Boustany, MD, MPH1, Achintya Singh, MD1, Anoosha Tauquir, 3, Hassan M. Shaheen, MD1, Jagriti Nahata, MD4, Asif Hitawala, MD5, Ashraf Almomani, MD1
1Cleveland Clinic Foundation, Cleveland, OH; 2OU-HCOM Cleveland, Waite Hill, OH; 3Cleveland Clinic, Fairview Park, OH; 4Maulana Azad Medical College, Delhi, Delhi, India; 5National Institutes of Health, Bethesda, MD
Introduction: Flood syndrome is a rare complication of patients with end-stage liver cirrhosis characterized by coinciding ventral hernia with spontaneous umbilical hernia rupture and extrusion of ascitic fluid through the defect. We present a unique case of Flood syndrome in a patient with decompensated cirrhosis and umbilical hernia.
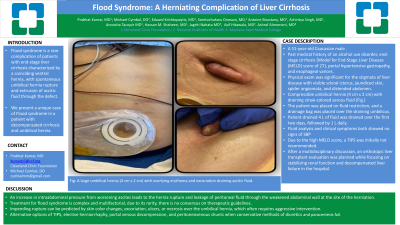
Case Description/Methods: A 51-year-old Caucasian male with a past medical history of an alcohol use disorder, end-stage cirrhosis [Model for End-Stage Liver Disease (MELD) score of 27], portal hypertensive gastropathy, and esophageal varices was presented to the hospital after noticing gushing of an around a liter of fluid through his umbilicus. Physical exam was significant for the stigmata of liver disease with visible scleral icterus, jaundiced skin, spider angiomata, and distended abdomen. Also evident was a compressible umbilical hernia (4 cm x 2 cm) with draining straw-colored serous fluid (Figure). The patient was placed on fluid restriction, and a drainage bag was placed over the draining umbilicus. A total of 4 liters of fluid was drained from his umbilicus for the first two days of admission, which decreased to 1 liter daily by day four of his hospitalization. Fluid analysis of the ascitic fluid did not show any evidence of spontaneous bacterial peritonitis. Due to the high MELD score, a transjugular intrahepatic portosystemic shunting procedure (TIPS) was initially not recommended. After a multidisciplinary discussion, an orthotopic liver transplant evaluation was planned while focusing on stabilizing renal function and decompensated liver failure in the hospital.
Discussion: An increase in intraabdominal pressure from worsening ascites leads to the hernia rupture and ultimate leakage of peritoneal fluid through the weakened abdominal wall at the site of the herniation. Patients with end-stage liver disease and long-standing ascites are susceptible to the rare and potentially life-threatening flooding syndrome. Treatment for flood syndrome is complex and multifactorial. Due to its rarity, there is no consensus on therapeutic guidelines. However, an impending rupture can be predicted by skin color changes, excoriation, ulcers, or necrosis over the umbilical hernia, which often requires aggressive intervention. Physicians may attempt TIPS, elective herniorrhaphy, portal venous decompression, and peritoneovenous shunts as an alternative to failed conservative methods with diuretics and regular paracentesis.

Disclosures:
Prabhat Kumar, MD1, Michael M. Cymbal, BS2, Eduard Krishtopaytis, MD1, Somtochukwu Onwuzo, MD1, Antoine Boustany, MD, MPH1, Achintya Singh, MD1, Anoosha Tauquir, 3, Hassan M. Shaheen, MD1, Jagriti Nahata, MD4, Asif Hitawala, MD5, Ashraf Almomani, MD1. E0521 - Flood Syndrome: A Herniating Complication of Liver Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Cleveland Clinic Foundation, Cleveland, OH; 2OU-HCOM Cleveland, Waite Hill, OH; 3Cleveland Clinic, Fairview Park, OH; 4Maulana Azad Medical College, Delhi, Delhi, India; 5National Institutes of Health, Bethesda, MD
Introduction: Flood syndrome is a rare complication of patients with end-stage liver cirrhosis characterized by coinciding ventral hernia with spontaneous umbilical hernia rupture and extrusion of ascitic fluid through the defect. We present a unique case of Flood syndrome in a patient with decompensated cirrhosis and umbilical hernia.
Case Description/Methods: A 51-year-old Caucasian male with a past medical history of an alcohol use disorder, end-stage cirrhosis [Model for End-Stage Liver Disease (MELD) score of 27], portal hypertensive gastropathy, and esophageal varices was presented to the hospital after noticing gushing of an around a liter of fluid through his umbilicus. Physical exam was significant for the stigmata of liver disease with visible scleral icterus, jaundiced skin, spider angiomata, and distended abdomen. Also evident was a compressible umbilical hernia (4 cm x 2 cm) with draining straw-colored serous fluid (Figure). The patient was placed on fluid restriction, and a drainage bag was placed over the draining umbilicus. A total of 4 liters of fluid was drained from his umbilicus for the first two days of admission, which decreased to 1 liter daily by day four of his hospitalization. Fluid analysis of the ascitic fluid did not show any evidence of spontaneous bacterial peritonitis. Due to the high MELD score, a transjugular intrahepatic portosystemic shunting procedure (TIPS) was initially not recommended. After a multidisciplinary discussion, an orthotopic liver transplant evaluation was planned while focusing on stabilizing renal function and decompensated liver failure in the hospital.
Discussion: An increase in intraabdominal pressure from worsening ascites leads to the hernia rupture and ultimate leakage of peritoneal fluid through the weakened abdominal wall at the site of the herniation. Patients with end-stage liver disease and long-standing ascites are susceptible to the rare and potentially life-threatening flooding syndrome. Treatment for flood syndrome is complex and multifactorial. Due to its rarity, there is no consensus on therapeutic guidelines. However, an impending rupture can be predicted by skin color changes, excoriation, ulcers, or necrosis over the umbilical hernia, which often requires aggressive intervention. Physicians may attempt TIPS, elective herniorrhaphy, portal venous decompression, and peritoneovenous shunts as an alternative to failed conservative methods with diuretics and regular paracentesis.

Figure: A large umbilical hernia (4 cm x 2 cm) with overlying erythema and excoriation draining ascitic fluid.
Disclosures:
Prabhat Kumar indicated no relevant financial relationships.
Michael Cymbal indicated no relevant financial relationships.
Eduard Krishtopaytis indicated no relevant financial relationships.
Somtochukwu Onwuzo indicated no relevant financial relationships.
Antoine Boustany indicated no relevant financial relationships.
Achintya Singh indicated no relevant financial relationships.
Anoosha Tauquir indicated no relevant financial relationships.
Hassan Shaheen indicated no relevant financial relationships.
Jagriti Nahata indicated no relevant financial relationships.
Asif Hitawala indicated no relevant financial relationships.
Ashraf Almomani indicated no relevant financial relationships.
Prabhat Kumar, MD1, Michael M. Cymbal, BS2, Eduard Krishtopaytis, MD1, Somtochukwu Onwuzo, MD1, Antoine Boustany, MD, MPH1, Achintya Singh, MD1, Anoosha Tauquir, 3, Hassan M. Shaheen, MD1, Jagriti Nahata, MD4, Asif Hitawala, MD5, Ashraf Almomani, MD1. E0521 - Flood Syndrome: A Herniating Complication of Liver Cirrhosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
