Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0326 - If It Bleeds, It Leads: Endoscopic Presentation of Hemosuccus Pancreaticus
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Shahana Prakash, MD
University of Iowa Hospitals and Clinics
Iowa City, IA
Presenting Author(s)
Shahana Prakash, MD, Charles Meade, MD
University of Iowa Hospitals and Clinics, Iowa City, IA
Introduction: A 65 year old male presented as a transfer for further evaluation of multifactorial shock. Pertinent medical comorbidities included active alcohol use disorder and mild alcohol associated hepatitis. On OSH presentation, he was treated for multifactorial shock in setting of new atrial fibrillation with rapid ventricular response and MSSA bacteremia, and was subsequently transferred to our facility.
Case Description/Methods: On arrival, he had been started on systemic anticoagulation in light of his new diagnosis of atrial fibrillation and had downtrending hemoglobin from previously normal baseline ~15 to a nadir of 7-8. Several episodes of witnessed melena were documented, and the gastroenterology service was consulted. He had no known prior history of GI bleeding or cirrhosis.
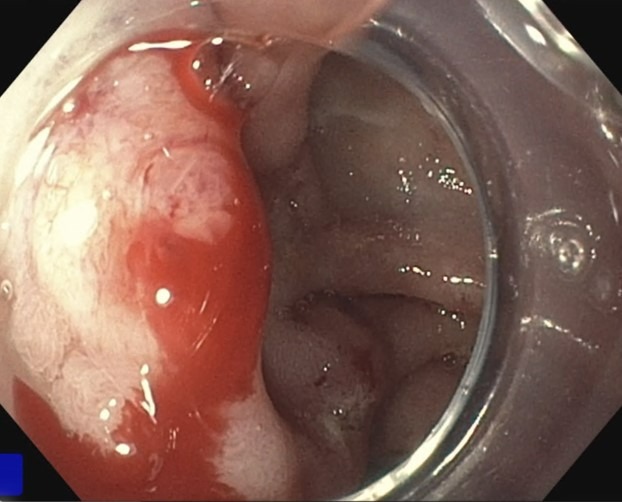
Endoscopic evaluation noted a small amount of hematin in the stomach without concerning source lesions. Examination of the duodenum was initially only notable for scant fresh red blood and small, clean based ulcers thought secondary to recent hypotension and ischemia. On prolonged examination of the duodenum intermittent fresh blood was observed originating from the ampulla, consistent with a diagnosis of hemosuccus pancreaticus.
Follow up dedicated CT angiography showed a thrombosed aneurysm in the pancreatic head, abutting the distal main pancreatic duct, that was concerning for the likely source lesion. The patient and family were offered interventional radiology intervention, but instead opted for hospice placement.
Discussion: Hemosuccus pancreaticus is typically associated with pancreatic pathology that ultimately causes luminal bleeding via erosion of pancreatic blood vessels in communication with the pancreatic duct. The source of bleeding is often an arterial aneurysm or pseudoaneurysm and associated bleeding can be severe and life-threatening. Active hemorrhage from the duodenal ampulla is a rare endoscopic finding and bleeding in cases of hemosuccus pancreaticus is frequently intermittent. In patients with obscure upper GI bleeding and the appropriate risk factors, a high index of suspicion is required to ultimately make the diagnosis.
Given the frequency of associated vascular abnormalities, all patients with suspected or confirmed hemosuccus pancreaticus merit dedicated vascular imaging and if a vascular lesion is identified, angiography and coil embolization are the preferred definitive management.
Disclosures:
Shahana Prakash, MD, Charles Meade, MD. B0326 - If It Bleeds, It Leads: Endoscopic Presentation of Hemosuccus Pancreaticus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Iowa Hospitals and Clinics, Iowa City, IA
Introduction: A 65 year old male presented as a transfer for further evaluation of multifactorial shock. Pertinent medical comorbidities included active alcohol use disorder and mild alcohol associated hepatitis. On OSH presentation, he was treated for multifactorial shock in setting of new atrial fibrillation with rapid ventricular response and MSSA bacteremia, and was subsequently transferred to our facility.
Case Description/Methods: On arrival, he had been started on systemic anticoagulation in light of his new diagnosis of atrial fibrillation and had downtrending hemoglobin from previously normal baseline ~15 to a nadir of 7-8. Several episodes of witnessed melena were documented, and the gastroenterology service was consulted. He had no known prior history of GI bleeding or cirrhosis.
Endoscopic evaluation noted a small amount of hematin in the stomach without concerning source lesions. Examination of the duodenum was initially only notable for scant fresh red blood and small, clean based ulcers thought secondary to recent hypotension and ischemia. On prolonged examination of the duodenum intermittent fresh blood was observed originating from the ampulla, consistent with a diagnosis of hemosuccus pancreaticus.
Follow up dedicated CT angiography showed a thrombosed aneurysm in the pancreatic head, abutting the distal main pancreatic duct, that was concerning for the likely source lesion. The patient and family were offered interventional radiology intervention, but instead opted for hospice placement.
Discussion: Hemosuccus pancreaticus is typically associated with pancreatic pathology that ultimately causes luminal bleeding via erosion of pancreatic blood vessels in communication with the pancreatic duct. The source of bleeding is often an arterial aneurysm or pseudoaneurysm and associated bleeding can be severe and life-threatening. Active hemorrhage from the duodenal ampulla is a rare endoscopic finding and bleeding in cases of hemosuccus pancreaticus is frequently intermittent. In patients with obscure upper GI bleeding and the appropriate risk factors, a high index of suspicion is required to ultimately make the diagnosis.
Given the frequency of associated vascular abnormalities, all patients with suspected or confirmed hemosuccus pancreaticus merit dedicated vascular imaging and if a vascular lesion is identified, angiography and coil embolization are the preferred definitive management.
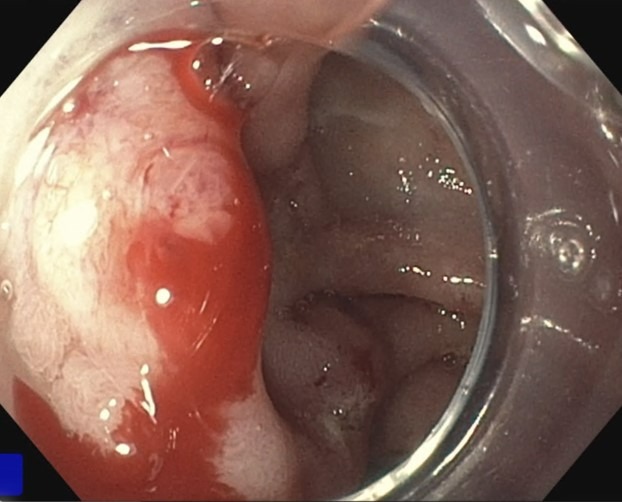
Figure: Intermittent active bleeding from ampulla consistent with endoscopic diagnosis of hemosuccus pancreaticus
Disclosures:
Shahana Prakash indicated no relevant financial relationships.
Charles Meade indicated no relevant financial relationships.
Shahana Prakash, MD, Charles Meade, MD. B0326 - If It Bleeds, It Leads: Endoscopic Presentation of Hemosuccus Pancreaticus, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
