Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0590 - Secondary HLH: Why Didn’t I Think of That First?
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- JC
Jessica Corder, MD
Naval Medical Center Portsmouth
Portsmouth, VA
Presenting Author(s)
Jessica Corder, MD, Daniel Shields, DO, Brett Sadowski, MD
Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare disease hallmarked by widespread immune activation ultimately leading to multi-organ failure. HLH occurs in two subsets: primary, typically with onset in childhood, and secondary, that occurs in response to another disease process. Given its rarity and nonspecific protean manifestations, the diagnosis of secondary HLH hinges heavily on excluding other more common diagnoses, a high index of suspicion, and interpretation of lab data. Our case highlights the workup and therapeutic dilemma in diagnosing HLH in a previously healthy 52-year-old male.
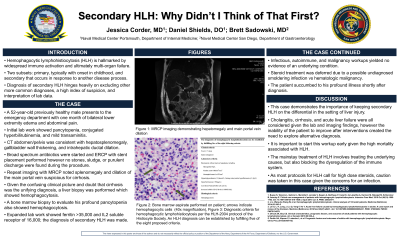
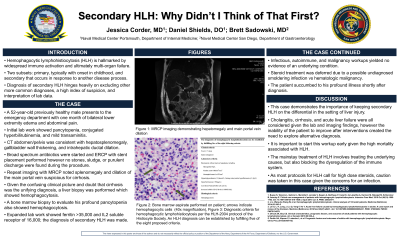
Case Description/Methods: A 52-year-old healthy male presented to the emergency department with the concern of leg swelling and vague abdominal pain. Initial lab work up was significant for WBC 1.56, Hgb 9.2, platelets 94, conjugated hyperbilirubinemia, AST 154 and ALT 99. CT abdomen/pelvis showed hepatosplenomegaly, gallbladder wall thickening, and intrahepatic ductal dilation. Initial concerns included cholangitis which prompted broad spectrum antibiotics and ERCP with stent placement, though no stones, sludge, or purulent discharge were found. MRCP noted splenomegaly and dilation of the main portal vein suspicious for cirrhosis. Given the confusing clinical picture and doubt that cirrhosis was the unifying diagnosis, a liver biopsy was performed which showed significant hemophagocytosis. Given this finding, in addition to a ferritin >35,000 and IL2 soluble receptor of 16,000, a diagnosis of secondary HLH was made. Steroid treatment was deferred due to a possible undiagnosed smoldering infection and concern for possible relapse with induction vs obscuring the diagnosis of some underlying hematologic malignancy. He was transferred to a quaternary institution where he succumbed to his profound illness a few days post transfer.
Discussion: This case demonstrates the importance of keeping secondary HLH on the differential in the setting of liver injury. Cholangitis, cirrhosis, and acute liver failure were all considered given the lab and imaging findings, however the inability of the patient to improve after interventions created the need to explore alternative diagnosis. This prompted the consideration and ultimately led to the diagnosis of secondary HLH. The mainstay treatment of HLH involves treating the underlying causes, but also blocking the dysregulation of the immune system. As most protocols for HLH call for high dose steroids, caution was taken in this case given the concerns for an infection.
Disclosures:
Jessica Corder, MD, Daniel Shields, DO, Brett Sadowski, MD. E0590 - Secondary HLH: Why Didn’t I Think of That First?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Naval Medical Center Portsmouth, Portsmouth, VA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare disease hallmarked by widespread immune activation ultimately leading to multi-organ failure. HLH occurs in two subsets: primary, typically with onset in childhood, and secondary, that occurs in response to another disease process. Given its rarity and nonspecific protean manifestations, the diagnosis of secondary HLH hinges heavily on excluding other more common diagnoses, a high index of suspicion, and interpretation of lab data. Our case highlights the workup and therapeutic dilemma in diagnosing HLH in a previously healthy 52-year-old male.
Case Description/Methods: A 52-year-old healthy male presented to the emergency department with the concern of leg swelling and vague abdominal pain. Initial lab work up was significant for WBC 1.56, Hgb 9.2, platelets 94, conjugated hyperbilirubinemia, AST 154 and ALT 99. CT abdomen/pelvis showed hepatosplenomegaly, gallbladder wall thickening, and intrahepatic ductal dilation. Initial concerns included cholangitis which prompted broad spectrum antibiotics and ERCP with stent placement, though no stones, sludge, or purulent discharge were found. MRCP noted splenomegaly and dilation of the main portal vein suspicious for cirrhosis. Given the confusing clinical picture and doubt that cirrhosis was the unifying diagnosis, a liver biopsy was performed which showed significant hemophagocytosis. Given this finding, in addition to a ferritin >35,000 and IL2 soluble receptor of 16,000, a diagnosis of secondary HLH was made. Steroid treatment was deferred due to a possible undiagnosed smoldering infection and concern for possible relapse with induction vs obscuring the diagnosis of some underlying hematologic malignancy. He was transferred to a quaternary institution where he succumbed to his profound illness a few days post transfer.
Discussion: This case demonstrates the importance of keeping secondary HLH on the differential in the setting of liver injury. Cholangitis, cirrhosis, and acute liver failure were all considered given the lab and imaging findings, however the inability of the patient to improve after interventions created the need to explore alternative diagnosis. This prompted the consideration and ultimately led to the diagnosis of secondary HLH. The mainstay treatment of HLH involves treating the underlying causes, but also blocking the dysregulation of the immune system. As most protocols for HLH call for high dose steroids, caution was taken in this case given the concerns for an infection.
Disclosures:
Jessica Corder indicated no relevant financial relationships.
Daniel Shields indicated no relevant financial relationships.
Brett Sadowski indicated no relevant financial relationships.
Jessica Corder, MD, Daniel Shields, DO, Brett Sadowski, MD. E0590 - Secondary HLH: Why Didn’t I Think of That First?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

