Back

Poster Session E - Tuesday Afternoon
Category: Liver
E0604 - An Intrahepatic Portosystemic Shunt Masquerading as a Tumor
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Dayana Nasr, MD
SUNY Upstate University Hospital
Syracuse, NY
Presenting Author(s)
Dayana Nasr, MD1, Pujitha Kudaravalli, MBBS2, Vishnu Kumar, MD3, Alyssa Ionno, MD2, Janane Nasr, MD4, Ganesh Aswath, MD2, Savio John, MD2
1SUNY Upstate University Hospital, Syracuse, NY; 2State University of New York Upstate University Hospital, Syracuse, NY; 3SUNY Upstate Medical University, Syracuse, NY; 4Lebanese American University, Beirut, Beyrouth, Lebanon
Introduction: Portosystemic shunts can be congenital or acquired and are divided into extrahepatic and intrahepatic shunts. Intrahepatic portosystemic venous shunts (IPSVSs) are abnormal intrahepatic connections that occur between branches of the portal vein (PV) and hepatic veins (HV) or IVC. Patients with IPSVSs can be symptomatic or asymptomatic as most of the cases are detected incidentally on imaging. However, they can potentially lead to long term complications by allowing bypass of mesenteric venous return into systemic circulation without going through the liver. We herein describe the case of a 58-year-old woman who was incidentally found to have an IPSVS on imaging for which she was recommended periodic surveillance imaging.
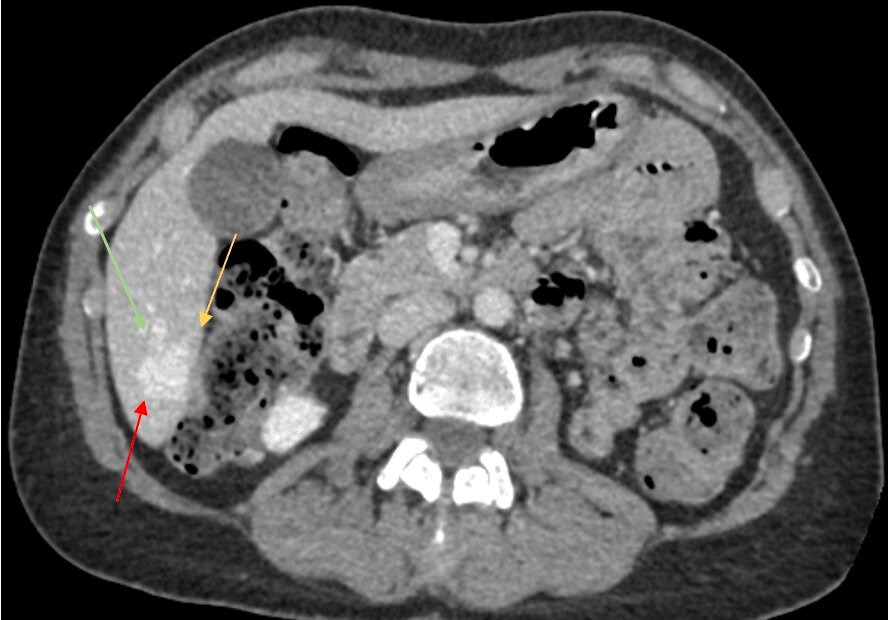
Case Description/Methods: A 58-year-old woman was undergoing workup for weight loss and was noted to have a 2.3 x 2.0 cm hyperdense nodular lesion in the posterior segment of the right hepatic lobe suspicious for hemangioma or a hypervascular neoplasm on CT abdomen pelvis. She was referred to the hepatobiliary clinic and a CTA abdomen pelvis was then performed and showed a lobulated 2.2 x 2.1 x 2.9 cm lesion in segment 6 consistent with an intrahepatic portosystemic shunt (figure 1). The patient was otherwise asymptomatic and therefore was advised to continue with periodic imaging surveillance.
Discussion: IPSVSs are divided into 4 types depending on their morphology. In type 1, a single large vessel connects the PV or its right branch to the IVC. Type 2 involves a localized peripheral shunt within one hepatic segment that has one or more communications between peripheral branches of the PV and HV. In type 3, an aneurysmal connection exists between PV and HV. And finally, multiple communications between PV and HV in multiple lobes are present in type 4. In patients without a history of liver disease or trauma, the origin of the IPSVS is presumed to be congenital. CT scan, MRI and even color Doppler sonograms should provide visualizations of the feeding portal vein and draining hepatic vein. For symptomatic IPSVSs, endovascular closure is the standard of care. However, no consensus exists for asymptomatic cases and surveillance is an appropriate option in asymptomatic patients.
Disclosures:
Dayana Nasr, MD1, Pujitha Kudaravalli, MBBS2, Vishnu Kumar, MD3, Alyssa Ionno, MD2, Janane Nasr, MD4, Ganesh Aswath, MD2, Savio John, MD2. E0604 - An Intrahepatic Portosystemic Shunt Masquerading as a Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1SUNY Upstate University Hospital, Syracuse, NY; 2State University of New York Upstate University Hospital, Syracuse, NY; 3SUNY Upstate Medical University, Syracuse, NY; 4Lebanese American University, Beirut, Beyrouth, Lebanon
Introduction: Portosystemic shunts can be congenital or acquired and are divided into extrahepatic and intrahepatic shunts. Intrahepatic portosystemic venous shunts (IPSVSs) are abnormal intrahepatic connections that occur between branches of the portal vein (PV) and hepatic veins (HV) or IVC. Patients with IPSVSs can be symptomatic or asymptomatic as most of the cases are detected incidentally on imaging. However, they can potentially lead to long term complications by allowing bypass of mesenteric venous return into systemic circulation without going through the liver. We herein describe the case of a 58-year-old woman who was incidentally found to have an IPSVS on imaging for which she was recommended periodic surveillance imaging.
Case Description/Methods: A 58-year-old woman was undergoing workup for weight loss and was noted to have a 2.3 x 2.0 cm hyperdense nodular lesion in the posterior segment of the right hepatic lobe suspicious for hemangioma or a hypervascular neoplasm on CT abdomen pelvis. She was referred to the hepatobiliary clinic and a CTA abdomen pelvis was then performed and showed a lobulated 2.2 x 2.1 x 2.9 cm lesion in segment 6 consistent with an intrahepatic portosystemic shunt (figure 1). The patient was otherwise asymptomatic and therefore was advised to continue with periodic imaging surveillance.
Discussion: IPSVSs are divided into 4 types depending on their morphology. In type 1, a single large vessel connects the PV or its right branch to the IVC. Type 2 involves a localized peripheral shunt within one hepatic segment that has one or more communications between peripheral branches of the PV and HV. In type 3, an aneurysmal connection exists between PV and HV. And finally, multiple communications between PV and HV in multiple lobes are present in type 4. In patients without a history of liver disease or trauma, the origin of the IPSVS is presumed to be congenital. CT scan, MRI and even color Doppler sonograms should provide visualizations of the feeding portal vein and draining hepatic vein. For symptomatic IPSVSs, endovascular closure is the standard of care. However, no consensus exists for asymptomatic cases and surveillance is an appropriate option in asymptomatic patients.
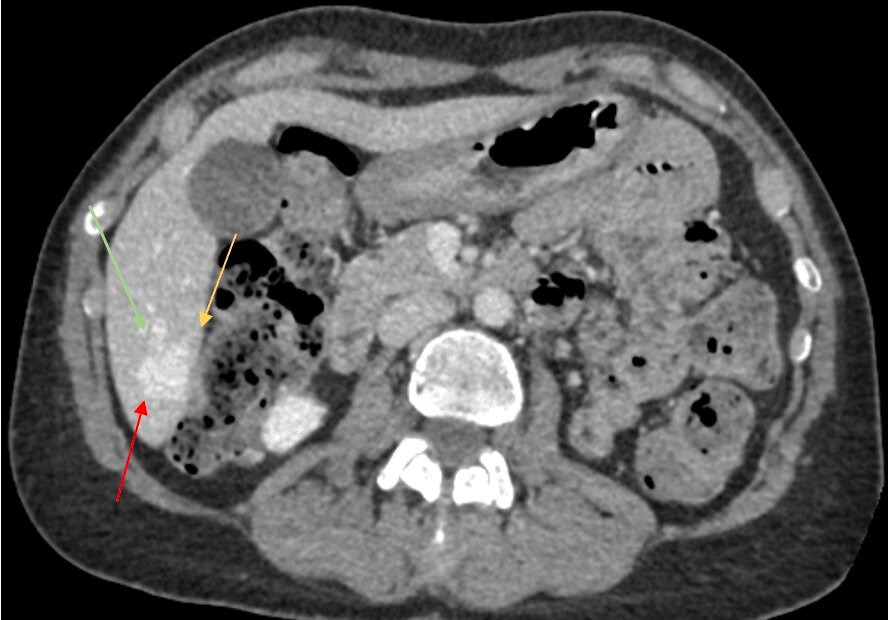
Figure: Axial CTA abdomen venous phase showing aneurysmal communication (red arrow) between right portal vein (yellow arrow) and middle hepatic vein (green arrow) in segment 6 of the liver
Disclosures:
Dayana Nasr indicated no relevant financial relationships.
Pujitha Kudaravalli indicated no relevant financial relationships.
Vishnu Kumar indicated no relevant financial relationships.
Alyssa Ionno indicated no relevant financial relationships.
Janane Nasr indicated no relevant financial relationships.
Ganesh Aswath indicated no relevant financial relationships.
Savio John indicated no relevant financial relationships.
Dayana Nasr, MD1, Pujitha Kudaravalli, MBBS2, Vishnu Kumar, MD3, Alyssa Ionno, MD2, Janane Nasr, MD4, Ganesh Aswath, MD2, Savio John, MD2. E0604 - An Intrahepatic Portosystemic Shunt Masquerading as a Tumor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
