Back

Poster Session E - Tuesday Afternoon
Category: Small Intestine
E0645 - A Rare Case of Gastrointestinal Amyloidosis Due to Monoclonal Gammopathy of Undetermined Significance
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sarah Singh, MD
West Virginia University - Camden Clark Medical Center
Parkersburg, WV
Presenting Author(s)
Sarah Singh, MD, Guru Gopireddy, MD, Scott Naum, DO, Michael Iannetti, MD
West Virginia University - Camden Clark Medical Center, Parkersburg, WV
Introduction: Amyloidosis of the gastrointestinal (GI) tract is an uncommon disorder caused by extracellular deposition of fibrils made up of a variety of serum proteins. Symptomatic GI amyloidosis presents with one of four syndromes: GI bleeding, malabsorption, protein-losing gastroenteropathy, or GI dysmotility. Diagnosis of GI amyloidosis requires a tissue biopsy with positive Congo red staining or the presence of amyloid fibrils on electron microscopy. The prognosis of patients with amyloidosis and GI involvement appears to be worse than those without.
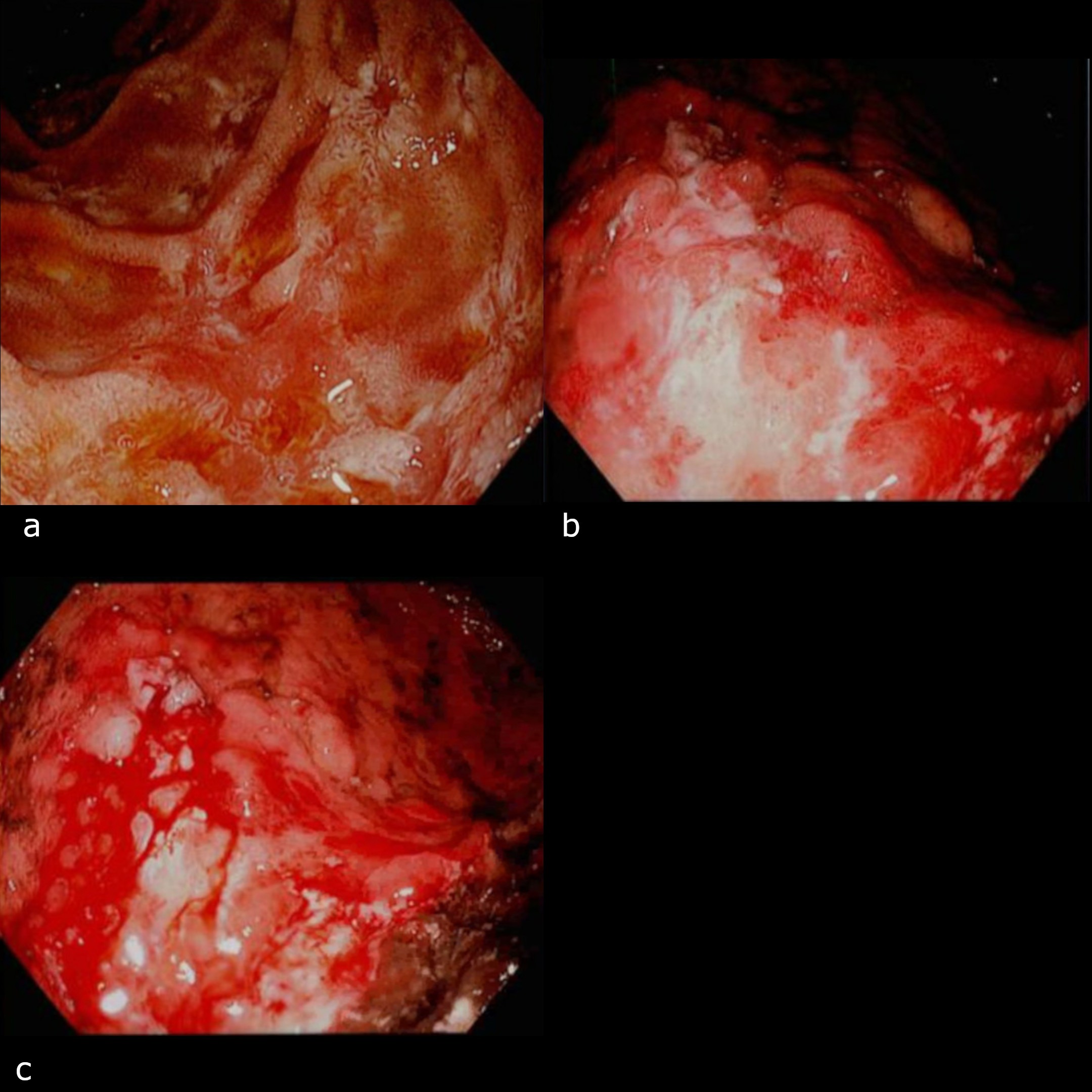
Case Description/Methods: A 64-year-old female with a past medical history significant for hypertension, systolic heart failure, depression, hyperlipidemia, and hypothyroidism presented with right lower quadrant abdominal pain. On examination, her lungs were clear, abdomen was benign, and vitals were stable. CT scan of the abdomen showed evidence of mesenteric, upper abdominal, and retroperitoneal adenopathy as well as omental findings concerning for metastatic disease or carcinomatosis. An EGD with biopsy revealed multiple gastric and duodenal ulcers.
She presented five months later with hematemesis, weight loss, melanotic stool, and abdominal pain. EGD revealed findings suggestive of gastric malignancy involving the body and cardia of the stomach. CA 125 and LDH levels were elevated with increased adenopathy in the chest. Biopsy of gastric mucosa and duodenum showed findings suggestive of amyloidosis, with AL (Kappa) type amyloid deposition and positive Congo red staining. Kappa chain was detected in urine and serum as well, suggesting multiorgan involvement. Bone marrow biopsy revealed findings consistent with MGUS. A PET/CT demonstrated moderate irregular gastric wall thickening and infiltration of the omental fat with concern for intraperitoneal spread. She was started on CyBorD nine months after initial presentation. She died at home one month later.
Discussion: Case reports concerning GI amyloidosis have reported on multiple myeloma, MGUS, or were not associated with a plasma cell dyscrasia. Two other case reports presented with MGUS at different stages, from an incidental finding to advanced disease with severe complications such as hematemesis, anemia, and weight loss. Four of these six patients improved with treatment while another two succumbed to the disease. This case illustrates that, while rare, it is important for clinicians to be aware of GI amyloidosis as early diagnosis is imperative for effective treatment and prognosis.
Disclosures:
Sarah Singh, MD, Guru Gopireddy, MD, Scott Naum, DO, Michael Iannetti, MD. E0645 - A Rare Case of Gastrointestinal Amyloidosis Due to Monoclonal Gammopathy of Undetermined Significance, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
West Virginia University - Camden Clark Medical Center, Parkersburg, WV
Introduction: Amyloidosis of the gastrointestinal (GI) tract is an uncommon disorder caused by extracellular deposition of fibrils made up of a variety of serum proteins. Symptomatic GI amyloidosis presents with one of four syndromes: GI bleeding, malabsorption, protein-losing gastroenteropathy, or GI dysmotility. Diagnosis of GI amyloidosis requires a tissue biopsy with positive Congo red staining or the presence of amyloid fibrils on electron microscopy. The prognosis of patients with amyloidosis and GI involvement appears to be worse than those without.
Case Description/Methods: A 64-year-old female with a past medical history significant for hypertension, systolic heart failure, depression, hyperlipidemia, and hypothyroidism presented with right lower quadrant abdominal pain. On examination, her lungs were clear, abdomen was benign, and vitals were stable. CT scan of the abdomen showed evidence of mesenteric, upper abdominal, and retroperitoneal adenopathy as well as omental findings concerning for metastatic disease or carcinomatosis. An EGD with biopsy revealed multiple gastric and duodenal ulcers.
She presented five months later with hematemesis, weight loss, melanotic stool, and abdominal pain. EGD revealed findings suggestive of gastric malignancy involving the body and cardia of the stomach. CA 125 and LDH levels were elevated with increased adenopathy in the chest. Biopsy of gastric mucosa and duodenum showed findings suggestive of amyloidosis, with AL (Kappa) type amyloid deposition and positive Congo red staining. Kappa chain was detected in urine and serum as well, suggesting multiorgan involvement. Bone marrow biopsy revealed findings consistent with MGUS. A PET/CT demonstrated moderate irregular gastric wall thickening and infiltration of the omental fat with concern for intraperitoneal spread. She was started on CyBorD nine months after initial presentation. She died at home one month later.
Discussion: Case reports concerning GI amyloidosis have reported on multiple myeloma, MGUS, or were not associated with a plasma cell dyscrasia. Two other case reports presented with MGUS at different stages, from an incidental finding to advanced disease with severe complications such as hematemesis, anemia, and weight loss. Four of these six patients improved with treatment while another two succumbed to the disease. This case illustrates that, while rare, it is important for clinicians to be aware of GI amyloidosis as early diagnosis is imperative for effective treatment and prognosis.
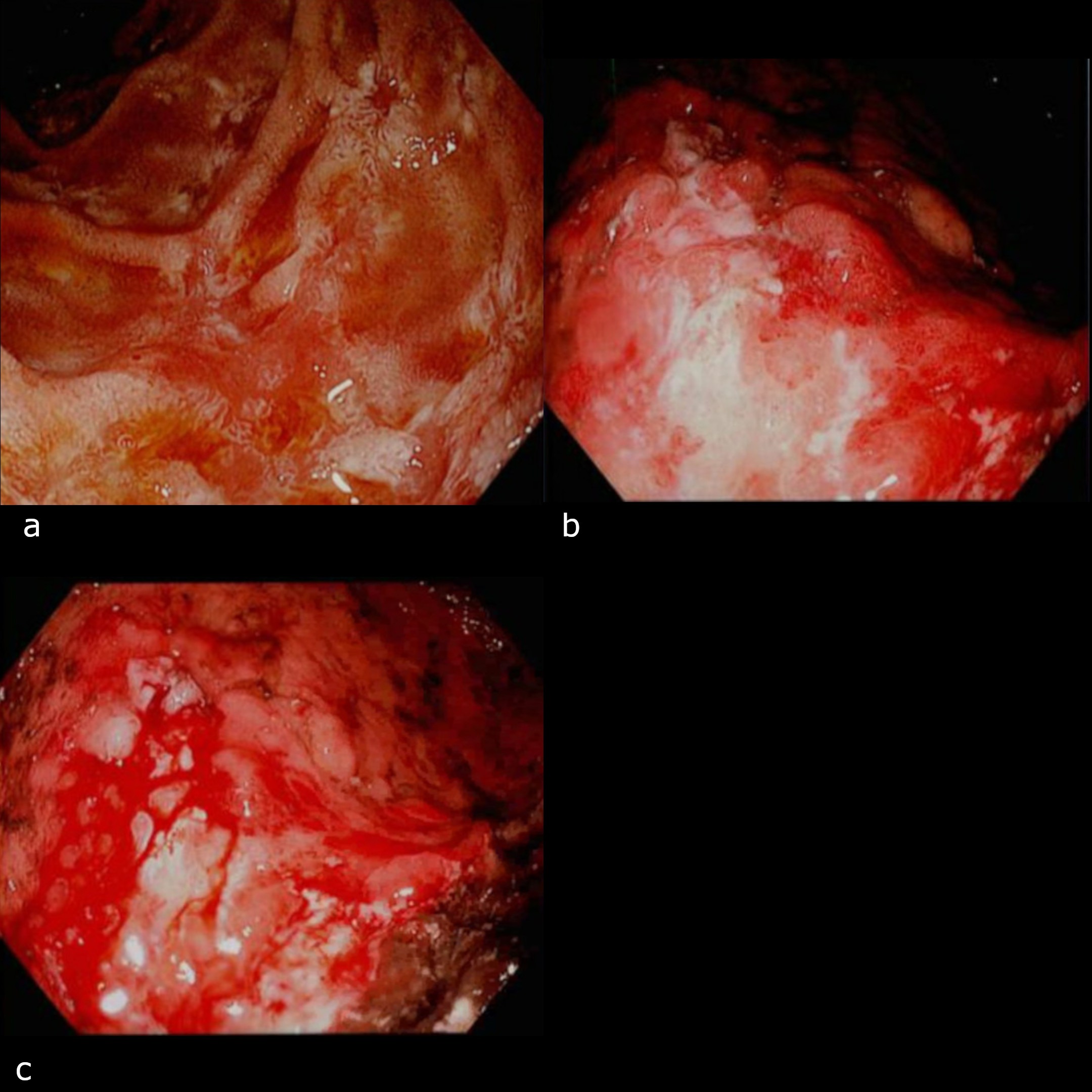
Figure: (a) Lining of the first part of the duodenum. (b-c) Active duodenitis in the first and second portions of the duodenum
Disclosures:
Sarah Singh indicated no relevant financial relationships.
Guru Gopireddy indicated no relevant financial relationships.
Scott Naum indicated no relevant financial relationships.
Michael Iannetti indicated no relevant financial relationships.
Sarah Singh, MD, Guru Gopireddy, MD, Scott Naum, DO, Michael Iannetti, MD. E0645 - A Rare Case of Gastrointestinal Amyloidosis Due to Monoclonal Gammopathy of Undetermined Significance, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
