Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0692 - Inpatient Mortality of PEG Tube Placement in High-Risk Patients
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Suvithan Rajadurai, MD
The Warren Alpert Medical School of Brown University
Providence, RI
Presenting Author(s)
William Hogan, MD1, Suvithan Rajadurai, MD1, Sivamainthan Vithiananthan, MD2, Alan H. Daniels, MD3
1The Warren Alpert Medical School of Brown University, Providence, RI; 2Cambridge Health Alliance, Cambridge, MA; 3Rhode Island Hospital & The Miriam Hospital, Providence, RI
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are used as access for long-term enteral feedings in many clinical situations. Some are predisposed to poorer clinical outcomes especially in high in-house mortality. The purpose of this investigation was to use a nationwide sample of inpatients with PEG tubes to identify comorbidities associated with in-hospital mortality.
Methods: We conducted a retrospective cohort study identifying patients with PEG tube placement registered in the Nationwide Inpatient Sample (NIS) database from 2009-2014. Patient records with ICD-9-CM code for PEG placement were identified. The Elixhauser Comorbidity Index (ECI) was applied to each patient record to group patients by the Index’s common comorbidities. Demographic analysis included age, race, sex, income, and hospital. Frequently associated diagnoses in the records were identified and used as proxy to suggest PEG tube placement purpose.
Results: 1,087,994 patients with PEG tube placement were examined. The mean age was 67.7 years. Fifty-four percent were male, and 46% were female. 51% presented to urban non-teaching institutions, 43% to urban teaching institutions, and 6% to rural institutions. The majority of patients were identified as White (63%). Common diagnoses, aside from PEG tube placement, included neurologic infarct or hemorrhage (25.8%), hearing loss (14.7%), food/vomit pneumonitis (11.6%), acute respiratory failure (5.4%), acute kidney failure (3.7%), pneumonia (2.6%), UTI (2.4%), dysphagia (1.9%), and dehydration (1.9%).
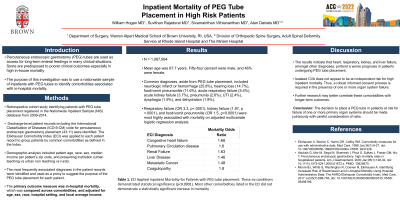
Respiratory failure (OR 3.3, p< .0001), kidney failure (1.87, p < .0001), and food/vomit pneumonitis (OR 1.5, p< 0.0001) were most highly associated with mortality on adjusted multivariate logistic regression analysis. Using the ECI, inpatient mortality was significantly increased for patients with concomitant congestive heart failure (OR 1.68, p< 0.0001), pulmonary circulation disease (1.60, p< 0.0001), renal failure (1.63, p< 0.0001), liver disease (1.46, p< 0.0001), metastatic cancer (1.48, p< 0.0001), and coagulopathy (1.80, p< 0.0001).
Discussion: The results indicate that individual organ failure portends a worse prognosis in patients undergoing PEG tube placement with high inpatient mortality. Isolated CVA does not appear to be an independent risk for high inpatient mortality. Thus, a robust informed consent process is required in the presence of one or more organ system failure. Further research may better correlate these comorbidities with longer-term outcomes.
Disclosures:
William Hogan, MD1, Suvithan Rajadurai, MD1, Sivamainthan Vithiananthan, MD2, Alan H. Daniels, MD3. E0692 - Inpatient Mortality of PEG Tube Placement in High-Risk Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1The Warren Alpert Medical School of Brown University, Providence, RI; 2Cambridge Health Alliance, Cambridge, MA; 3Rhode Island Hospital & The Miriam Hospital, Providence, RI
Introduction: Percutaneous endoscopic gastrostomy (PEG) tubes are used as access for long-term enteral feedings in many clinical situations. Some are predisposed to poorer clinical outcomes especially in high in-house mortality. The purpose of this investigation was to use a nationwide sample of inpatients with PEG tubes to identify comorbidities associated with in-hospital mortality.
Methods: We conducted a retrospective cohort study identifying patients with PEG tube placement registered in the Nationwide Inpatient Sample (NIS) database from 2009-2014. Patient records with ICD-9-CM code for PEG placement were identified. The Elixhauser Comorbidity Index (ECI) was applied to each patient record to group patients by the Index’s common comorbidities. Demographic analysis included age, race, sex, income, and hospital. Frequently associated diagnoses in the records were identified and used as proxy to suggest PEG tube placement purpose.
Results: 1,087,994 patients with PEG tube placement were examined. The mean age was 67.7 years. Fifty-four percent were male, and 46% were female. 51% presented to urban non-teaching institutions, 43% to urban teaching institutions, and 6% to rural institutions. The majority of patients were identified as White (63%). Common diagnoses, aside from PEG tube placement, included neurologic infarct or hemorrhage (25.8%), hearing loss (14.7%), food/vomit pneumonitis (11.6%), acute respiratory failure (5.4%), acute kidney failure (3.7%), pneumonia (2.6%), UTI (2.4%), dysphagia (1.9%), and dehydration (1.9%).
Respiratory failure (OR 3.3, p< .0001), kidney failure (1.87, p < .0001), and food/vomit pneumonitis (OR 1.5, p< 0.0001) were most highly associated with mortality on adjusted multivariate logistic regression analysis. Using the ECI, inpatient mortality was significantly increased for patients with concomitant congestive heart failure (OR 1.68, p< 0.0001), pulmonary circulation disease (1.60, p< 0.0001), renal failure (1.63, p< 0.0001), liver disease (1.46, p< 0.0001), metastatic cancer (1.48, p< 0.0001), and coagulopathy (1.80, p< 0.0001).
Discussion: The results indicate that individual organ failure portends a worse prognosis in patients undergoing PEG tube placement with high inpatient mortality. Isolated CVA does not appear to be an independent risk for high inpatient mortality. Thus, a robust informed consent process is required in the presence of one or more organ system failure. Further research may better correlate these comorbidities with longer-term outcomes.
Disclosures:
William Hogan indicated no relevant financial relationships.
Suvithan Rajadurai indicated no relevant financial relationships.
Sivamainthan Vithiananthan indicated no relevant financial relationships.
Alan Daniels indicated no relevant financial relationships.
William Hogan, MD1, Suvithan Rajadurai, MD1, Sivamainthan Vithiananthan, MD2, Alan H. Daniels, MD3. E0692 - Inpatient Mortality of PEG Tube Placement in High-Risk Patients, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
