Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0731 - The Use of Endoscopic Band Ligation for the Management of Gastric Antral Vascular Ectasia (GAVE)
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Romy Chamoun, MD
Lankenau Medical Center
Wynnewood, PA
Presenting Author(s)
Romy Chamoun, MD, Ashley Manganiello, MD, Roy Taoutel, MD, Bryan Stone, DO, Bob Etemad, MD
Lankenau Medical Center, Wynnewood, PA
Introduction: Gastric antral vascular ectasia (GAVE), also known as watermelon stomach due to its endoscopic appearance, is characterized by ectatic mucosal vessels in the gastric antrum. . The clinical presentation is similar to that of portal hypertensive gastropathy (PHG) with chronic slow GI blood loss. Though associated with cirrhosis, unlike PHG it is not caused by portal hypertension. These lesions are typically flat, linear, red stripes and so the diagnosis and treatment are based on this classic appearance which may be confirmed on biopsy. Serial treatments with argon plasma coagulation can reduce transfusion requirements and restore hemoglobin levels in these patients. Below we present a case of nodular GAVE, a rare variant, which requires a high level of clinical suspicion for appropriate and timely therapy.
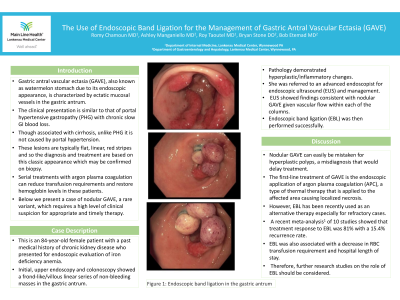
Case Description/Methods: This is an 84-year-old female patient with a past medical history of chronic kidney disease who presented for endoscopic evaluation of iron deficiency anemia. Initial, upper endoscopy and colonoscopy showed a frond-like/villous linear series of non-bleeding masses in the gastric antrum. Pathology demonstrated hyperplastic/inflammatory changes. She was referred to an advanced endoscopist for endoscopic ultrasound (EUS) and management. EUS showed findings consistent with nodular GAVE given vascular flow within each of the columns. Endoscopic band ligation (EBL) was then performed successfully.
Discussion: Nodular GAVE can easily be mistaken for hyperplastic polyps, a misdiagnosis that would delay treatment. The first-line treatment of GAVE is the endoscopic application of argon plasma coagulation (APC), a type of thermal therapy that is applied to the affected area causing localized necrosis. However, EBL has been recently used as an alternative therapy especially for refractory cases. A recent meta-analysis1 of 10 studies showed that treatment response to EBL was 81% with a 15.4% recurrence rate. EBL was also associated with a decrease in RBC transfusion requirement and hospital length of stay. Therefore, further research studies on the role of EBL should be considered.
1. Mohan BP, Toy G, Kassab LL, Ponnada S, Chandan S, Parbhu S, Chandna S, Adler DG. Endoscopic band ligation in the treatment of gastric antral vascular ectasia: a systematic review and meta-analysis. Gastrointest Endosc. 2021 Dec;94(6):1021-1029.e10. doi: 10.1016/j.gie.2021.08.017. Epub 2021 Sep 1. PMID: 34480922.

Disclosures:
Romy Chamoun, MD, Ashley Manganiello, MD, Roy Taoutel, MD, Bryan Stone, DO, Bob Etemad, MD. E0731 - The Use of Endoscopic Band Ligation for the Management of Gastric Antral Vascular Ectasia (GAVE), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Lankenau Medical Center, Wynnewood, PA
Introduction: Gastric antral vascular ectasia (GAVE), also known as watermelon stomach due to its endoscopic appearance, is characterized by ectatic mucosal vessels in the gastric antrum. . The clinical presentation is similar to that of portal hypertensive gastropathy (PHG) with chronic slow GI blood loss. Though associated with cirrhosis, unlike PHG it is not caused by portal hypertension. These lesions are typically flat, linear, red stripes and so the diagnosis and treatment are based on this classic appearance which may be confirmed on biopsy. Serial treatments with argon plasma coagulation can reduce transfusion requirements and restore hemoglobin levels in these patients. Below we present a case of nodular GAVE, a rare variant, which requires a high level of clinical suspicion for appropriate and timely therapy.
Case Description/Methods: This is an 84-year-old female patient with a past medical history of chronic kidney disease who presented for endoscopic evaluation of iron deficiency anemia. Initial, upper endoscopy and colonoscopy showed a frond-like/villous linear series of non-bleeding masses in the gastric antrum. Pathology demonstrated hyperplastic/inflammatory changes. She was referred to an advanced endoscopist for endoscopic ultrasound (EUS) and management. EUS showed findings consistent with nodular GAVE given vascular flow within each of the columns. Endoscopic band ligation (EBL) was then performed successfully.
Discussion: Nodular GAVE can easily be mistaken for hyperplastic polyps, a misdiagnosis that would delay treatment. The first-line treatment of GAVE is the endoscopic application of argon plasma coagulation (APC), a type of thermal therapy that is applied to the affected area causing localized necrosis. However, EBL has been recently used as an alternative therapy especially for refractory cases. A recent meta-analysis1 of 10 studies showed that treatment response to EBL was 81% with a 15.4% recurrence rate. EBL was also associated with a decrease in RBC transfusion requirement and hospital length of stay. Therefore, further research studies on the role of EBL should be considered.
1. Mohan BP, Toy G, Kassab LL, Ponnada S, Chandan S, Parbhu S, Chandna S, Adler DG. Endoscopic band ligation in the treatment of gastric antral vascular ectasia: a systematic review and meta-analysis. Gastrointest Endosc. 2021 Dec;94(6):1021-1029.e10. doi: 10.1016/j.gie.2021.08.017. Epub 2021 Sep 1. PMID: 34480922.

Figure: Endoscopic band ligation in the gastric antrum
Disclosures:
Romy Chamoun indicated no relevant financial relationships.
Ashley Manganiello indicated no relevant financial relationships.
Roy Taoutel indicated no relevant financial relationships.
Bryan Stone indicated no relevant financial relationships.
Bob Etemad indicated no relevant financial relationships.
Romy Chamoun, MD, Ashley Manganiello, MD, Roy Taoutel, MD, Bryan Stone, DO, Bob Etemad, MD. E0731 - The Use of Endoscopic Band Ligation for the Management of Gastric Antral Vascular Ectasia (GAVE), ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
