Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0721 - Russel Body Gastritis: When the Rare Meets the Odd
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Mahmoud Bayoumi, MD, MPH
University of Arizona College of Medicine
Phoenix, AZ
Presenting Author(s)
Mahmoud Bayoumi, MD, MPH, Renuka Pathi, MD, Brian M. Fung, MD, Kelly Zucker, DO, Hugo Pinillos, MD, FACG
University of Arizona College of Medicine, Phoenix, AZ
Introduction: The significance of chronic gastritis is underrated. Even though Helicobacter Pylori (HP) has been the main contributing factor to this condition, if testing for it comes back negative, we should always rule out other underlying diseases, especially if the biopsy reveals Russell body (RB) gastritis.
Case Description/Methods: A 67-year-old male with a past medical history of immune thrombocytopenic purpura (ITP) on prednisone and eltrombopag, hypertension, and choledocholithiasis status post cholecystectomy complicated by abscess formation and drain placement, presented with worsening nausea, vomiting, and abdominal pain for three days associated with early satiety and weight loss. His symptoms were not related to food or activity.
Vital signs and physical exam were unremarkable except for right upper quadrant abdominal tenderness. Labs were remarkable for WBC 55 k/ul, HGB 11 g/dl, and PLT 90 k/ul. Full infectious workup was negative. CT scan showed massive splenomegaly with widespread lymphadenopathy and circumferential wall thickening of the gastric fundus and body.
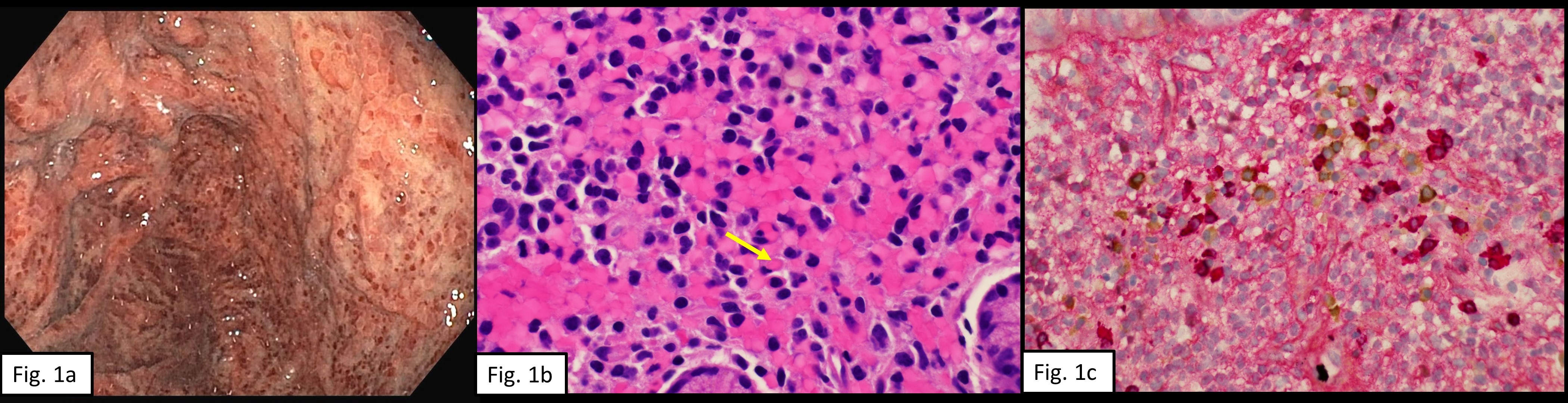
An upper endoscopy was performed and revealed diffuse gastric erythema in a mosaic pattern, most pronounced in the body of the stomach (Fig 1a). Biopsies were obtained from the gastric antrum and body. Gastric body biopsies revealed gastric oxyntic mucosa with RB gastritis (Fig 1b), and it was negative for HP, intestinal metaplasia, dysplasia, or malignancy. Kappa and lambda immunohistochemistry stain showed a polyclonal mixed population of plasma cells (Fig 1c), indicating no underlying malignancy.
HP stool antigen was checked twice, and it was negative.
His WBC continued to rise, and bone marrow (BM) biopsy was performed. Findings were suspicious for myelodysplastic/myeloproliferative disorder; however, a reactive process could not be ruled out.
Since the patient's condition significantly deteriorated, a repeat BM biopsy revealed morphological changes consistent with chronic myelomonocytic leukemia (CMML). After discussing goals of care with the patient, he opted for hospice care and expired after three days.
Discussion: RB gastritis is a reactive mucosal infiltration of plasma cells filled with cytoplasmic RB. There is a strong association with HP infection, but there is also an association with hematopoietic malignancies and gastric adenocarcinoma. Our case represents the vital importance of looking for underlying malignancies in HP negative RB gastritis patients.
Disclosures:
Mahmoud Bayoumi, MD, MPH, Renuka Pathi, MD, Brian M. Fung, MD, Kelly Zucker, DO, Hugo Pinillos, MD, FACG. E0721 - Russel Body Gastritis: When the Rare Meets the Odd, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix, AZ
Introduction: The significance of chronic gastritis is underrated. Even though Helicobacter Pylori (HP) has been the main contributing factor to this condition, if testing for it comes back negative, we should always rule out other underlying diseases, especially if the biopsy reveals Russell body (RB) gastritis.
Case Description/Methods: A 67-year-old male with a past medical history of immune thrombocytopenic purpura (ITP) on prednisone and eltrombopag, hypertension, and choledocholithiasis status post cholecystectomy complicated by abscess formation and drain placement, presented with worsening nausea, vomiting, and abdominal pain for three days associated with early satiety and weight loss. His symptoms were not related to food or activity.
Vital signs and physical exam were unremarkable except for right upper quadrant abdominal tenderness. Labs were remarkable for WBC 55 k/ul, HGB 11 g/dl, and PLT 90 k/ul. Full infectious workup was negative. CT scan showed massive splenomegaly with widespread lymphadenopathy and circumferential wall thickening of the gastric fundus and body.
An upper endoscopy was performed and revealed diffuse gastric erythema in a mosaic pattern, most pronounced in the body of the stomach (Fig 1a). Biopsies were obtained from the gastric antrum and body. Gastric body biopsies revealed gastric oxyntic mucosa with RB gastritis (Fig 1b), and it was negative for HP, intestinal metaplasia, dysplasia, or malignancy. Kappa and lambda immunohistochemistry stain showed a polyclonal mixed population of plasma cells (Fig 1c), indicating no underlying malignancy.
HP stool antigen was checked twice, and it was negative.
His WBC continued to rise, and bone marrow (BM) biopsy was performed. Findings were suspicious for myelodysplastic/myeloproliferative disorder; however, a reactive process could not be ruled out.
Since the patient's condition significantly deteriorated, a repeat BM biopsy revealed morphological changes consistent with chronic myelomonocytic leukemia (CMML). After discussing goals of care with the patient, he opted for hospice care and expired after three days.
Discussion: RB gastritis is a reactive mucosal infiltration of plasma cells filled with cytoplasmic RB. There is a strong association with HP infection, but there is also an association with hematopoietic malignancies and gastric adenocarcinoma. Our case represents the vital importance of looking for underlying malignancies in HP negative RB gastritis patients.
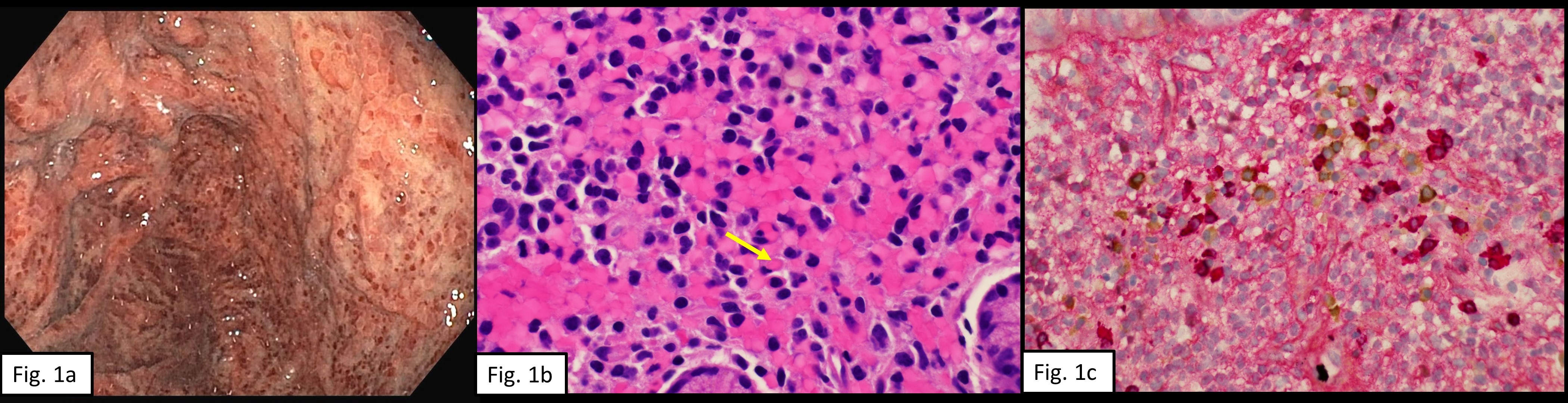
Figure: Figure 1a. An upper endoscopy showing diffuse punctuate gastric erythema with mucosal mosaic pattern.
Figure 1b. A high power stomach biopsy with Hematoxylin and Eosin stain showing atypical plasma cells with Russell bodies (yellow arrow) which are eosinophilic homogeneous immunoglobulin-containing inclusions.
Figure 1c. A high power stomach biopsy with kappa and lambda immunohistochemistry stain showing polyclonal mixed population of plasma cells (positive for both kappa and lambda).
Figure 1b. A high power stomach biopsy with Hematoxylin and Eosin stain showing atypical plasma cells with Russell bodies (yellow arrow) which are eosinophilic homogeneous immunoglobulin-containing inclusions.
Figure 1c. A high power stomach biopsy with kappa and lambda immunohistochemistry stain showing polyclonal mixed population of plasma cells (positive for both kappa and lambda).
Disclosures:
Mahmoud Bayoumi indicated no relevant financial relationships.
Renuka Pathi indicated no relevant financial relationships.
Brian Fung indicated no relevant financial relationships.
Kelly Zucker indicated no relevant financial relationships.
Hugo Pinillos indicated no relevant financial relationships.
Mahmoud Bayoumi, MD, MPH, Renuka Pathi, MD, Brian M. Fung, MD, Kelly Zucker, DO, Hugo Pinillos, MD, FACG. E0721 - Russel Body Gastritis: When the Rare Meets the Odd, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
