Back

Poster Session E - Tuesday Afternoon
Category: Stomach
E0725 - Gastric Syphilis: An Unusual Etiology of Melena in a Patient With AIDS
Tuesday, October 25, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Neelima Gaddipati, MD, MBA
University of Miami/Jackson Health System
Miami, Florida
Presenting Author(s)
Award: Presidential Poster Award
Neelima Gaddipati, MD, MBA1, Andrew R. Scheinberg, MD2, Satyapal Chahar, MD1, Daniel A. Sussman, MD3
1University of Miami/Jackson Health System, Miami, FL; 2University of Miami / Jackson Health System, Miami, FL; 3University of Miami, Miami, FL
Introduction: The incidence of primary and secondary syphilis has increased across the United States by 6.8% during 2019-20 alone. Gastrointestinal manifestations of syphilis are rarely described. We present a patient with acquired immunodeficiency syndrome (AIDS) and persistent anemia secondary to gastric erosions from Treponema pallidum infection.
Case Description/Methods: A 23 year-old man with AIDS, nonadherence to antiretrovirals, and recent genitourinary gonorrhea/chlamydia infections presented with three months of subjective weight loss and two days of diarrhea, varying between melenic stools and bright red blood per rectum. Two weeks prior, he presented with similar symptoms, anemia of 3.6 and underwent an esophagogastroduodenoscopy (EGD) demonstrating esophageal candidiasis with normal stomach and duodenum. Colonoscopy at the time demonstrated abnormal rectal mucosa with congestion, erythema, and deep ulcerations; biopsies were negative for CMV, HSV1, HSV2, and T. pallidum. He was discharged on oral fluconazole.
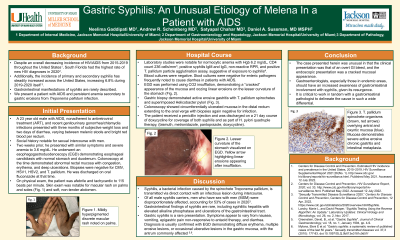
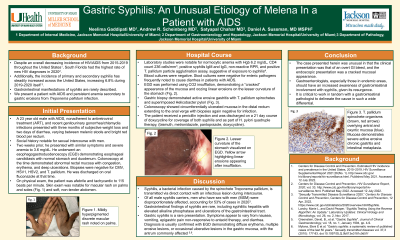
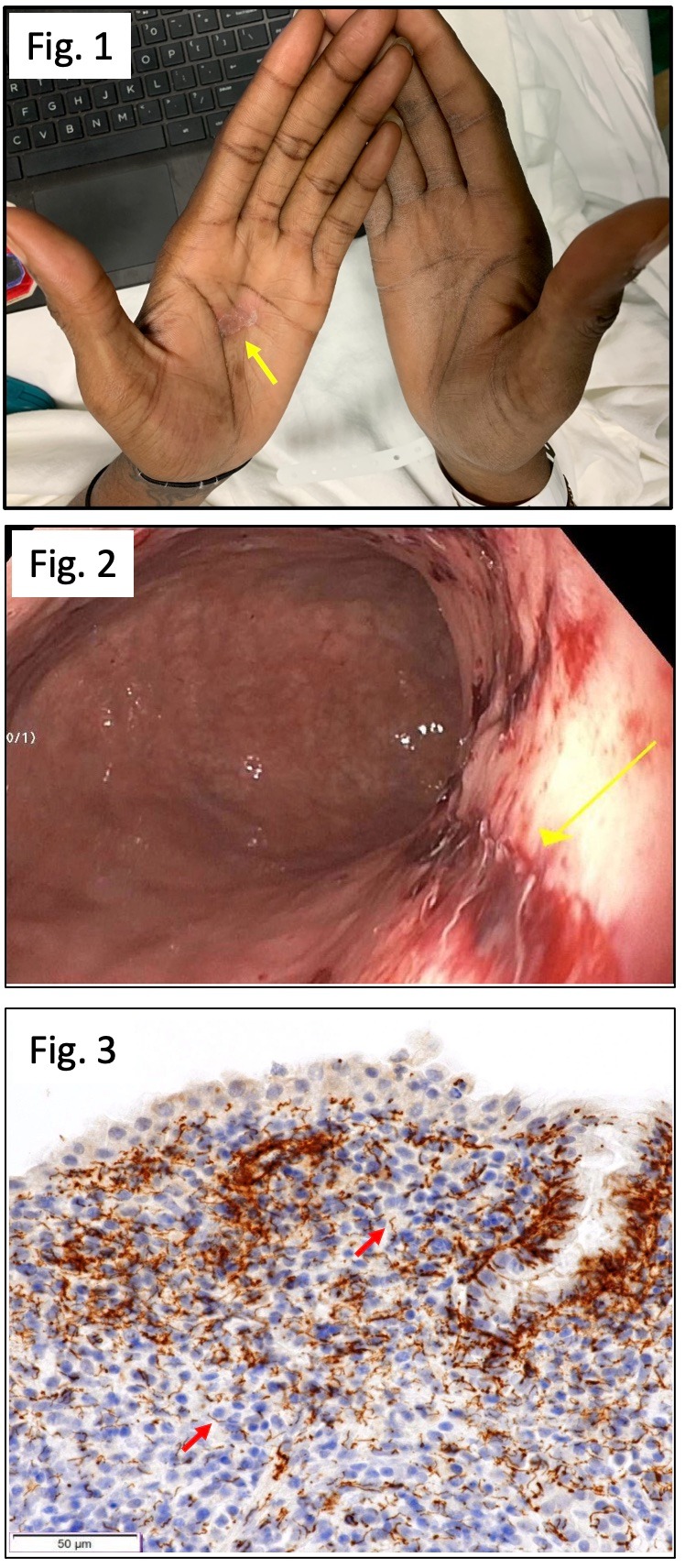
On readmission, he was afebrile and tachycardic to 115 beats per minute. Exam was notable for a discrete macular rash on palms and soles and soft, non-tender abdomen. Laboratory studies indicated normocytic anemia with Hgb 6.2. He had reactive T. pallidum antibodies, confirming syphilis. Blood and stool studies were negative for Campylobacter, Cryptosporidium, and other organisms noted to cause AIDS-related diarrhea. Repeat EGD was done, demonstrating a “cracked” appearance with insufflation of CO2 and oozing linear erosions on the lesser curvature of the stomach with gastric biopsy showing T. pallidum spirochetes with superimposed Helicobacter pylori. Colonoscopy showed circumferentially ulcerated mucosa in the distal rectum extending to the anal verge with biopsies again negative for infection including mycobacteria. He received a penicillin injection and was discharged on a 21 day course of doxycycline for late latent syphilis as well as H. pylori triple therapy.
Discussion: Gastric syphilis is rare, with patients having vague symptoms of nausea, vomiting, epigastric pain unrelieved by antacids, and diarrhea. Diagnosis can be confirmed with EGD demonstrating diffuse erythema, multiple erosive lesions, or ulcerative lesions in gastric mucosa. The case was unusual as the clinical presentation was an overt GI bleed, and the endoscopic presentation was a cracked mucosal appearance. Gastroenterologists should have an increased awareness of GI involvement with syphilis, given its resurgence.
Disclosures:
Neelima Gaddipati, MD, MBA1, Andrew R. Scheinberg, MD2, Satyapal Chahar, MD1, Daniel A. Sussman, MD3. E0725 - Gastric Syphilis: An Unusual Etiology of Melena in a Patient With AIDS, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Neelima Gaddipati, MD, MBA1, Andrew R. Scheinberg, MD2, Satyapal Chahar, MD1, Daniel A. Sussman, MD3
1University of Miami/Jackson Health System, Miami, FL; 2University of Miami / Jackson Health System, Miami, FL; 3University of Miami, Miami, FL
Introduction: The incidence of primary and secondary syphilis has increased across the United States by 6.8% during 2019-20 alone. Gastrointestinal manifestations of syphilis are rarely described. We present a patient with acquired immunodeficiency syndrome (AIDS) and persistent anemia secondary to gastric erosions from Treponema pallidum infection.
Case Description/Methods: A 23 year-old man with AIDS, nonadherence to antiretrovirals, and recent genitourinary gonorrhea/chlamydia infections presented with three months of subjective weight loss and two days of diarrhea, varying between melenic stools and bright red blood per rectum. Two weeks prior, he presented with similar symptoms, anemia of 3.6 and underwent an esophagogastroduodenoscopy (EGD) demonstrating esophageal candidiasis with normal stomach and duodenum. Colonoscopy at the time demonstrated abnormal rectal mucosa with congestion, erythema, and deep ulcerations; biopsies were negative for CMV, HSV1, HSV2, and T. pallidum. He was discharged on oral fluconazole.
On readmission, he was afebrile and tachycardic to 115 beats per minute. Exam was notable for a discrete macular rash on palms and soles and soft, non-tender abdomen. Laboratory studies indicated normocytic anemia with Hgb 6.2. He had reactive T. pallidum antibodies, confirming syphilis. Blood and stool studies were negative for Campylobacter, Cryptosporidium, and other organisms noted to cause AIDS-related diarrhea. Repeat EGD was done, demonstrating a “cracked” appearance with insufflation of CO2 and oozing linear erosions on the lesser curvature of the stomach with gastric biopsy showing T. pallidum spirochetes with superimposed Helicobacter pylori. Colonoscopy showed circumferentially ulcerated mucosa in the distal rectum extending to the anal verge with biopsies again negative for infection including mycobacteria. He received a penicillin injection and was discharged on a 21 day course of doxycycline for late latent syphilis as well as H. pylori triple therapy.
Discussion: Gastric syphilis is rare, with patients having vague symptoms of nausea, vomiting, epigastric pain unrelieved by antacids, and diarrhea. Diagnosis can be confirmed with EGD demonstrating diffuse erythema, multiple erosive lesions, or ulcerative lesions in gastric mucosa. The case was unusual as the clinical presentation was an overt GI bleed, and the endoscopic presentation was a cracked mucosal appearance. Gastroenterologists should have an increased awareness of GI involvement with syphilis, given its resurgence.
Figure: Fig.1: Macular rash on patient's palms.
Fig. 2: EGD image of linear erosions on the lesser curvature of the stomach.
Fig. 3: Arrows showing helically coiled spirochetes on Treponema pallidum immunohistochemical stain.
Fig. 2: EGD image of linear erosions on the lesser curvature of the stomach.
Fig. 3: Arrows showing helically coiled spirochetes on Treponema pallidum immunohistochemical stain.
Disclosures:
Neelima Gaddipati indicated no relevant financial relationships.
Andrew Scheinberg indicated no relevant financial relationships.
Satyapal Chahar indicated no relevant financial relationships.
Daniel Sussman indicated no relevant financial relationships.
Neelima Gaddipati, MD, MBA1, Andrew R. Scheinberg, MD2, Satyapal Chahar, MD1, Daniel A. Sussman, MD3. E0725 - Gastric Syphilis: An Unusual Etiology of Melena in a Patient With AIDS, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

