Back

Poster Session D - Tuesday Morning
Category: IBD
D0378 - Identifying Barriers to COVID-19 Vaccination in U.S. Veterans Who Have Inflammatory Bowel Disease
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Lakmal S. Ekanayake, DO
Wright State University Boonshoft School of Medicine
Centerville, OH
Presenting Author(s)
Lakmal S. Ekanayake, DO1, Shaina Ailawadi, BS (in-person presenter)2, Bahar Cheema, MD2, Ronald Markert, PhD2, Padmini Krishnamurthy, MD3
1Wright State University Boonshoft School of Medicine, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH; 3Dayton VA Medical Center, Dayton, OH
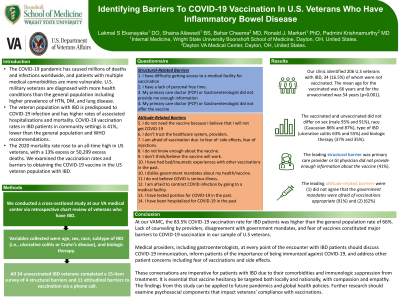
Introduction: The COVID-19 pandemic has caused millions of deaths and infections worldwide. Patients with multiple medical comorbidities are more vulnerable. Veterans have more health conditions than the general population with higher prevalence of HTN, DM, and lung disease. Veterans with IBD are predisposed to COVID-19 and have higher rates of associated hospitalizations and mortality. COVID-19 vaccination rates in IBD patients in community settings is 41%, lower than the general population and WHO recommendations. The 2020 veteran mortality rate rose to an all-time high, with a 13% increase or 50,299 excess deaths). We examined the rates of and barriers to COVID-19 vaccination in the veteran population with IBD.
Methods: We conducted a retrospective cross-sectional study at a VAMC. Data for demographics, subtype of IBD (i.e., ulcerative colitis or Crohn’s disease), and biologic therapy were collected. Unvaccinated veterans completed a 15-item survey of 4 structural barriers and 11 attitudinal barriers to vaccination via a phone call.
Results: We identified 206 veterans with IBD, 34 (16.5%) of whom were not vaccinated. Mean age for the vaccinated was 66 years and for the unvaccinated 54 years (p< 0.001). The two groups did not differ on sex (male 95% and 91%), race (Caucasian 86% and 87%), type of IBD (UC 63% and 55%), and biologic therapy (37% and 35%). The leading structural barrier was primary care provider or GI physician did not provide enough information about the vaccine(41%). The leading attitudinal barriers were (1) not agree that the government mandates were appropriate (91%) and (2) afraid of vaccinations (62%).
Discussion: The 83.5% COVID-19 vaccination rate for IBD patients was higher than the general population rate of 66%.1 Lack of provider counseling, disagree with government mandates, and fear of vaccines were major barriers. Due to their comorbidities and immunologic suppression from treatment, gastroenterologists managing IBD patients should discuss COVID-19 immunization including the importance of being immunized, fear of vaccines, and possible side effects. Vaccine hesitancy must be targeted locally and nationally, with compassion and empathy. Our findings can be applied to future pandemics and global health policies and be the basis for studies of psychosocial components that impact veterans’ compliance with vaccinations.
Disclosures:
Lakmal S. Ekanayake, DO1, Shaina Ailawadi, BS2, Bahar Cheema, MD2, Ronald Markert, PhD2, Padmini Krishnamurthy, MD3. D0378 - Identifying Barriers to COVID-19 Vaccination in U.S. Veterans Who Have Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wright State University Boonshoft School of Medicine, Centerville, OH; 2Wright State University Boonshoft School of Medicine, Dayton, OH; 3Dayton VA Medical Center, Dayton, OH
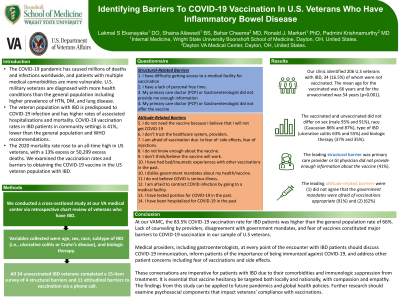
Introduction: The COVID-19 pandemic has caused millions of deaths and infections worldwide. Patients with multiple medical comorbidities are more vulnerable. Veterans have more health conditions than the general population with higher prevalence of HTN, DM, and lung disease. Veterans with IBD are predisposed to COVID-19 and have higher rates of associated hospitalizations and mortality. COVID-19 vaccination rates in IBD patients in community settings is 41%, lower than the general population and WHO recommendations. The 2020 veteran mortality rate rose to an all-time high, with a 13% increase or 50,299 excess deaths). We examined the rates of and barriers to COVID-19 vaccination in the veteran population with IBD.
Methods: We conducted a retrospective cross-sectional study at a VAMC. Data for demographics, subtype of IBD (i.e., ulcerative colitis or Crohn’s disease), and biologic therapy were collected. Unvaccinated veterans completed a 15-item survey of 4 structural barriers and 11 attitudinal barriers to vaccination via a phone call.
Results: We identified 206 veterans with IBD, 34 (16.5%) of whom were not vaccinated. Mean age for the vaccinated was 66 years and for the unvaccinated 54 years (p< 0.001). The two groups did not differ on sex (male 95% and 91%), race (Caucasian 86% and 87%), type of IBD (UC 63% and 55%), and biologic therapy (37% and 35%). The leading structural barrier was primary care provider or GI physician did not provide enough information about the vaccine(41%). The leading attitudinal barriers were (1) not agree that the government mandates were appropriate (91%) and (2) afraid of vaccinations (62%).
Discussion: The 83.5% COVID-19 vaccination rate for IBD patients was higher than the general population rate of 66%.1 Lack of provider counseling, disagree with government mandates, and fear of vaccines were major barriers. Due to their comorbidities and immunologic suppression from treatment, gastroenterologists managing IBD patients should discuss COVID-19 immunization including the importance of being immunized, fear of vaccines, and possible side effects. Vaccine hesitancy must be targeted locally and nationally, with compassion and empathy. Our findings can be applied to future pandemics and global health policies and be the basis for studies of psychosocial components that impact veterans’ compliance with vaccinations.
Disclosures:
Lakmal Ekanayake indicated no relevant financial relationships.
Shaina Ailawadi indicated no relevant financial relationships.
Bahar Cheema indicated no relevant financial relationships.
Ronald Markert indicated no relevant financial relationships.
Padmini Krishnamurthy indicated no relevant financial relationships.
Lakmal S. Ekanayake, DO1, Shaina Ailawadi, BS2, Bahar Cheema, MD2, Ronald Markert, PhD2, Padmini Krishnamurthy, MD3. D0378 - Identifying Barriers to COVID-19 Vaccination in U.S. Veterans Who Have Inflammatory Bowel Disease, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

