Back

Poster Session B - Monday Morning
Category: Colorectal Cancer Prevention
B0185 - Taking Caution at Road’s End: Incidental Finding of Appendiceal Goblet Cell Tumor on Colonoscopy
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kyler Kozacek, DO
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Award: Presidential Poster Award
Kyler Kozacek, DO, Ruth Reese, MD, Jeffrey Laczek, MD, Patrick Voorhees, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Appendiceal cancer is uncommon and rarely diagnosed on colonoscopy. We present a case of incidentally discovered goblet cell adenocarcinoma of the appendix and its subsequent management.
Case Description/Methods: 81-year-old male presented to GI clinic for persistent epigastric pain and reflux. Symptoms had been worsening for several years and were refractory to medical therapy. He denied unintentional weight loss, nausea, melena, or a family history of colorectal cancer. He had 9 colonoscopies between 1999 and 2016 for rectal bleeding due to hemorrhoids and diverticulosis, with a single 2mm TA removed in 2016 and 5-year follow-up advised. Repeat EGD and colonoscopy were scheduled, during which the appendiceal orifice (AO) had a “heaped-up” appearance and was biopsied with cold forceps. Histology revealed goblet cell adenocarcinoma (GCA.) CT of the abdomen and pelvis showed a mildly enlarged appendix, no LAD, and no evidence of metastasis. The patient underwent a laparoscopic right hemicolectomy. Pathology clarified that carcinoma extended from appendix to mesoappendix and cecum with extensive lymphovascular and perineural invasion. Resected margins and 19 resected lymph nodes were negative for malignancy and ultimately staged pT4aN0 (IIB). Colonoscopy 1 year later revealed healthy ileocolonic anastomosis without signs of polyps or other masses.
Discussion: Appendiceal cancer is categorized into two types: epithelial and neuroendocrine. GCA histologically has features of both. Incidence is rare, reportedly 0.05/100,000/year. It is usually an incidental finding following appendectomy for acute appendicitis and uncommonly found via colonoscopy. The AO is a key endoscopic landmark that should be identified on all colonoscopies to ensure completeness. Endoscopists should have a low threshold to biopsy abnormal-appearing tissue surrounding the AO. While no established risk factors for GCA, cases report an association with schistosomiasis and caucasian proclivity. Clinical diagnosis is difficult as presentations range from abdominal pain to appendicitis. Swift work-up and therapy are essential as appendiceal GCA can aggressively spread nodally or intraperitoneally. While evidence-based guidelines are not available, current management is similar to that of colon cancer with hemicolectomy for localized disease, adjuvant chemotherapy based on the surgical pathology, and post-treatment surveillance. We hope this case highlights the rarity of appendiceal GCA and the need for evidence-based guidelines.
Disclosures:
Kyler Kozacek, DO, Ruth Reese, MD, Jeffrey Laczek, MD, Patrick Voorhees, MD. B0185 - Taking Caution at Road’s End: Incidental Finding of Appendiceal Goblet Cell Tumor on Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Kyler Kozacek, DO, Ruth Reese, MD, Jeffrey Laczek, MD, Patrick Voorhees, MD
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Appendiceal cancer is uncommon and rarely diagnosed on colonoscopy. We present a case of incidentally discovered goblet cell adenocarcinoma of the appendix and its subsequent management.
Case Description/Methods: 81-year-old male presented to GI clinic for persistent epigastric pain and reflux. Symptoms had been worsening for several years and were refractory to medical therapy. He denied unintentional weight loss, nausea, melena, or a family history of colorectal cancer. He had 9 colonoscopies between 1999 and 2016 for rectal bleeding due to hemorrhoids and diverticulosis, with a single 2mm TA removed in 2016 and 5-year follow-up advised. Repeat EGD and colonoscopy were scheduled, during which the appendiceal orifice (AO) had a “heaped-up” appearance and was biopsied with cold forceps. Histology revealed goblet cell adenocarcinoma (GCA.) CT of the abdomen and pelvis showed a mildly enlarged appendix, no LAD, and no evidence of metastasis. The patient underwent a laparoscopic right hemicolectomy. Pathology clarified that carcinoma extended from appendix to mesoappendix and cecum with extensive lymphovascular and perineural invasion. Resected margins and 19 resected lymph nodes were negative for malignancy and ultimately staged pT4aN0 (IIB). Colonoscopy 1 year later revealed healthy ileocolonic anastomosis without signs of polyps or other masses.
Discussion: Appendiceal cancer is categorized into two types: epithelial and neuroendocrine. GCA histologically has features of both. Incidence is rare, reportedly 0.05/100,000/year. It is usually an incidental finding following appendectomy for acute appendicitis and uncommonly found via colonoscopy. The AO is a key endoscopic landmark that should be identified on all colonoscopies to ensure completeness. Endoscopists should have a low threshold to biopsy abnormal-appearing tissue surrounding the AO. While no established risk factors for GCA, cases report an association with schistosomiasis and caucasian proclivity. Clinical diagnosis is difficult as presentations range from abdominal pain to appendicitis. Swift work-up and therapy are essential as appendiceal GCA can aggressively spread nodally or intraperitoneally. While evidence-based guidelines are not available, current management is similar to that of colon cancer with hemicolectomy for localized disease, adjuvant chemotherapy based on the surgical pathology, and post-treatment surveillance. We hope this case highlights the rarity of appendiceal GCA and the need for evidence-based guidelines.
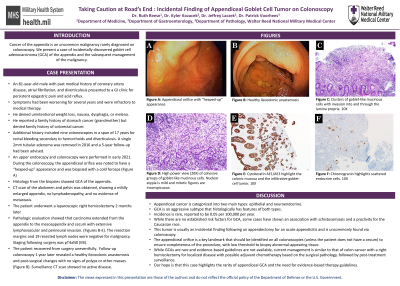
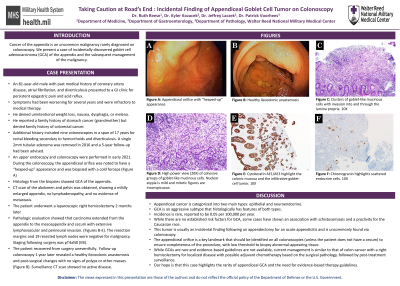
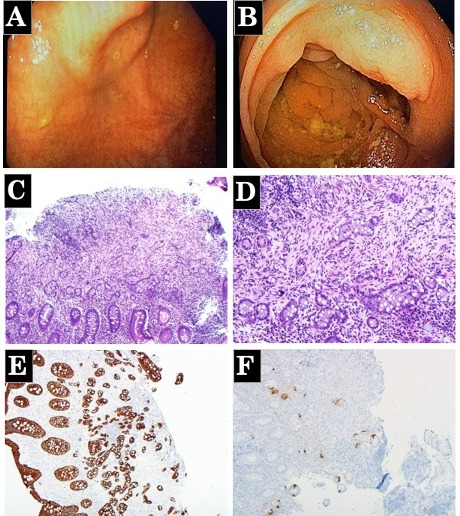
Figure: A) Appendiceal orifice with “heaped-up” appearance
B) Healthy ileocolonic anastamosis
C) Clusters of goblet-like mucinous cells with invasion into and through the lamina propria (10X)
D) High power view (20X) of cohesive groups of goblet-like mucinous cells. Nuclear atypia is mild and mitotic figures are inconspicuous
E) Cytokeratin AE1/AE3 highlights the colonic mucosa and the infiltrative goblet-cell tumor (10X)
F) Chromogranin highlights scattered endocrine cells (10X)
B) Healthy ileocolonic anastamosis
C) Clusters of goblet-like mucinous cells with invasion into and through the lamina propria (10X)
D) High power view (20X) of cohesive groups of goblet-like mucinous cells. Nuclear atypia is mild and mitotic figures are inconspicuous
E) Cytokeratin AE1/AE3 highlights the colonic mucosa and the infiltrative goblet-cell tumor (10X)
F) Chromogranin highlights scattered endocrine cells (10X)
Disclosures:
Kyler Kozacek indicated no relevant financial relationships.
Ruth Reese indicated no relevant financial relationships.
Jeffrey Laczek indicated no relevant financial relationships.
Patrick Voorhees indicated no relevant financial relationships.
Kyler Kozacek, DO, Ruth Reese, MD, Jeffrey Laczek, MD, Patrick Voorhees, MD. B0185 - Taking Caution at Road’s End: Incidental Finding of Appendiceal Goblet Cell Tumor on Colonoscopy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


