Back

Poster Session A - Sunday Afternoon
Category: Colon
A0122 - Dilemma of a Rectal Mass
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Raed Atiyat, MD
Saint MIchael's Medical Center
Paterson, NJ
Presenting Author(s)
Raed Atiyat, MD1, Siva Maruboyina, MD2, Kaveh Hajifathalian, MD, MPH3
1Saint MIchael's Medical Center, Paterson, NJ; 2Saint Michael's Medical Center, Newark, NJ; 3Rutgers New Jersey Medical School, Newark, NJ
Introduction:
Mucosal prolapsing polyps of the colon are uncommon findings during colonoscopy that are often misdiagnosed as malignant lesions that many times lead to unnecessary endoscopic and surgical resection. At times rectal prolapse/ mucosal prolapse syndrome can present as rectal submucosal mass similar to one another. Herein we present a case of a 63-year-old male with rectal prolapse that mimicked Submucosal rectal mass.
Case Description/Methods:
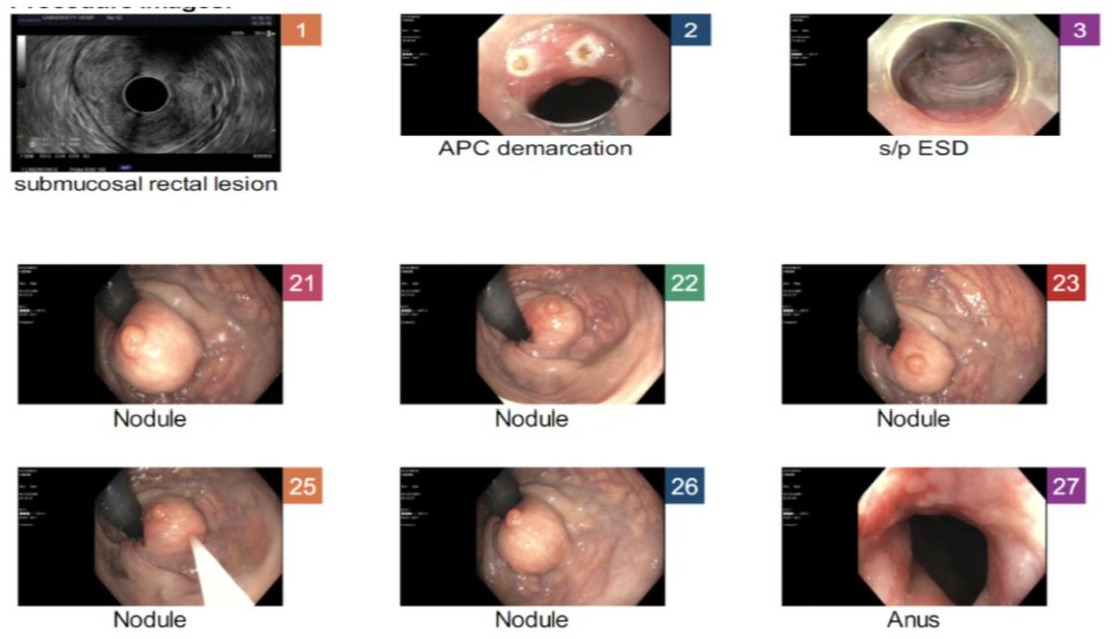
A 63-year-old male with prior medical history of hypertension, hyperlipidemia, obesity, treated Heliobacter pylori, hemorrhoids presented to the gastroenterology clinic due to 3-month history of dizziness, abdominal pain and bright red blood per rectum. Initial vitals were stable except for tachycardia. Physical examination was unremarkable except for external rectal hemorrhoids that were appreciated. Labs were also unremarkable on admission except for Normocytic anemia. Patient was planned and taken for colonoscopy which had poor bowel preparation, revealed large rectal mass, two small polyps in ascending and transverse colon which were resected. Patient was planned for flexible sigmoidoscopy and lower endoscopic ultrasound evaluation of rectal mass which revealed a hypoechoic, submucosal lesion measuring 14mm by 7mm. Patient underwent endoscopic submucosal resection of the rectal mass and removal of lesion. Post op he had rectal pain along with hypotension, which led patient to be admitted for overnight observation. On follow up patient complained of recurrent dizziness and BRBPR, sigmoidoscopy was planned and revealed superficial mucosal ulceration which was treated with bipolar cautery. Pathology of the rectal mass revealed largely denuded benign appearing congested polyp with granulation tissue and cautery artifacts. Patient’s symptoms improved on subsequent follow ups.
Discussion:
Mucosal prolapse presents as a common underlying mechanism rectal prolapse, inflammatory polyps, solitary rectal ulcer syndrome that were previously proposed to be grouped under the umbrella term “mucosal prolapse syndrome”. Mucosal prolapse can manifest as ulcerated, flat erythematous, or polypoid lesions. At times they can even mimic adenocarcinomas, adenomas both endoscopically and histologically. Most of the time rectal prolapses polyps have been seen in patients with mucosal prolapse syndrome. Thus, it is vital to differentiate and diagnose rectal prolapse versus true rectal mass in order to exclude malignancies. This will help guide management and surveillance strategy.
Disclosures:
Raed Atiyat, MD1, Siva Maruboyina, MD2, Kaveh Hajifathalian, MD, MPH3. A0122 - Dilemma of a Rectal Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Saint MIchael's Medical Center, Paterson, NJ; 2Saint Michael's Medical Center, Newark, NJ; 3Rutgers New Jersey Medical School, Newark, NJ
Introduction:
Mucosal prolapsing polyps of the colon are uncommon findings during colonoscopy that are often misdiagnosed as malignant lesions that many times lead to unnecessary endoscopic and surgical resection. At times rectal prolapse/ mucosal prolapse syndrome can present as rectal submucosal mass similar to one another. Herein we present a case of a 63-year-old male with rectal prolapse that mimicked Submucosal rectal mass.
Case Description/Methods:
A 63-year-old male with prior medical history of hypertension, hyperlipidemia, obesity, treated Heliobacter pylori, hemorrhoids presented to the gastroenterology clinic due to 3-month history of dizziness, abdominal pain and bright red blood per rectum. Initial vitals were stable except for tachycardia. Physical examination was unremarkable except for external rectal hemorrhoids that were appreciated. Labs were also unremarkable on admission except for Normocytic anemia. Patient was planned and taken for colonoscopy which had poor bowel preparation, revealed large rectal mass, two small polyps in ascending and transverse colon which were resected. Patient was planned for flexible sigmoidoscopy and lower endoscopic ultrasound evaluation of rectal mass which revealed a hypoechoic, submucosal lesion measuring 14mm by 7mm. Patient underwent endoscopic submucosal resection of the rectal mass and removal of lesion. Post op he had rectal pain along with hypotension, which led patient to be admitted for overnight observation. On follow up patient complained of recurrent dizziness and BRBPR, sigmoidoscopy was planned and revealed superficial mucosal ulceration which was treated with bipolar cautery. Pathology of the rectal mass revealed largely denuded benign appearing congested polyp with granulation tissue and cautery artifacts. Patient’s symptoms improved on subsequent follow ups.
Discussion:
Mucosal prolapse presents as a common underlying mechanism rectal prolapse, inflammatory polyps, solitary rectal ulcer syndrome that were previously proposed to be grouped under the umbrella term “mucosal prolapse syndrome”. Mucosal prolapse can manifest as ulcerated, flat erythematous, or polypoid lesions. At times they can even mimic adenocarcinomas, adenomas both endoscopically and histologically. Most of the time rectal prolapses polyps have been seen in patients with mucosal prolapse syndrome. Thus, it is vital to differentiate and diagnose rectal prolapse versus true rectal mass in order to exclude malignancies. This will help guide management and surveillance strategy.
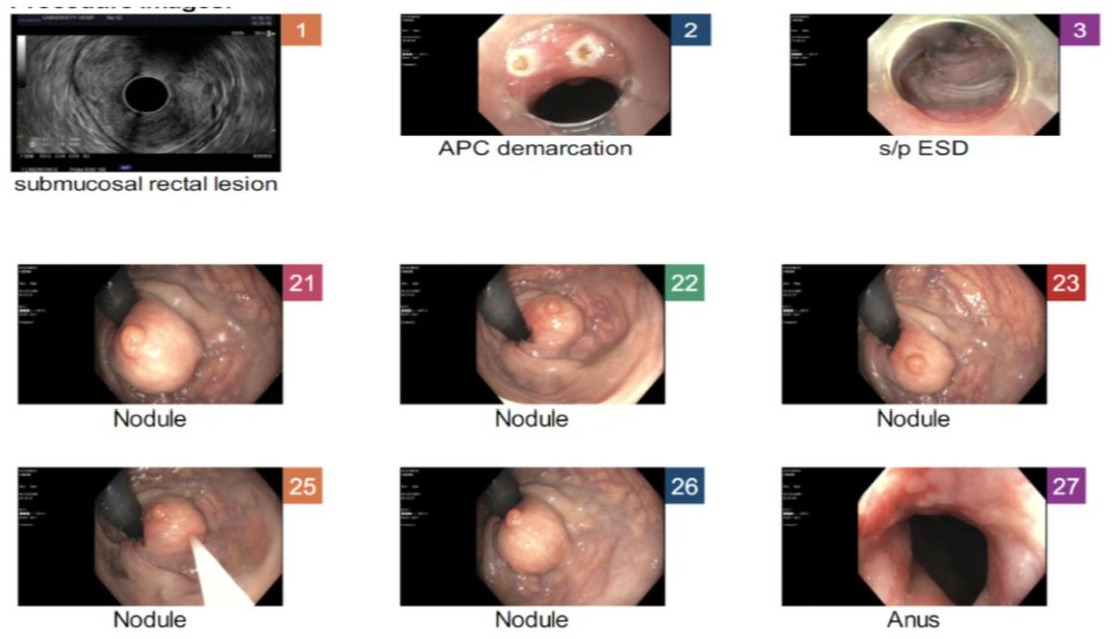
Figure: Nodules from Colonoscopy
Disclosures:
Raed Atiyat indicated no relevant financial relationships.
Siva Maruboyina indicated no relevant financial relationships.
Kaveh Hajifathalian indicated no relevant financial relationships.
Raed Atiyat, MD1, Siva Maruboyina, MD2, Kaveh Hajifathalian, MD, MPH3. A0122 - Dilemma of a Rectal Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
