Back

Poster Session C - Monday Afternoon
Category: Endoscopy Video Forum
C0198 - EUS-Guided Cyst Gastrostomy for Treatment of a Pancreatic Pseudocyst Extending Into the Mediastinum Resulting in Acute Respiratory Failure
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Alexandra Kimchy, DO
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Alexandra Kimchy, DO, William D. Davis, DO, Ahmad Nakshabandi, MD, Stanley Pietrak, MD, Walid Chalhoub, MD
MedStar Georgetown University Hospital, Washington, DC
Introduction: Mediastinal pseudocysts are the result of a rare drainage tract formation that develops more often in patients with a history of alcohol related chronic pancreatitis. The current evidence suggests favorable outcomes using endoscopic transmural drainage in the management of pancreatic pseudocysts. Here, we present a challenging approach to an unusual complication of a pancreatic pseudocyst extending into the mediastinum using EUS guided creation of a cyst gastrostomy.
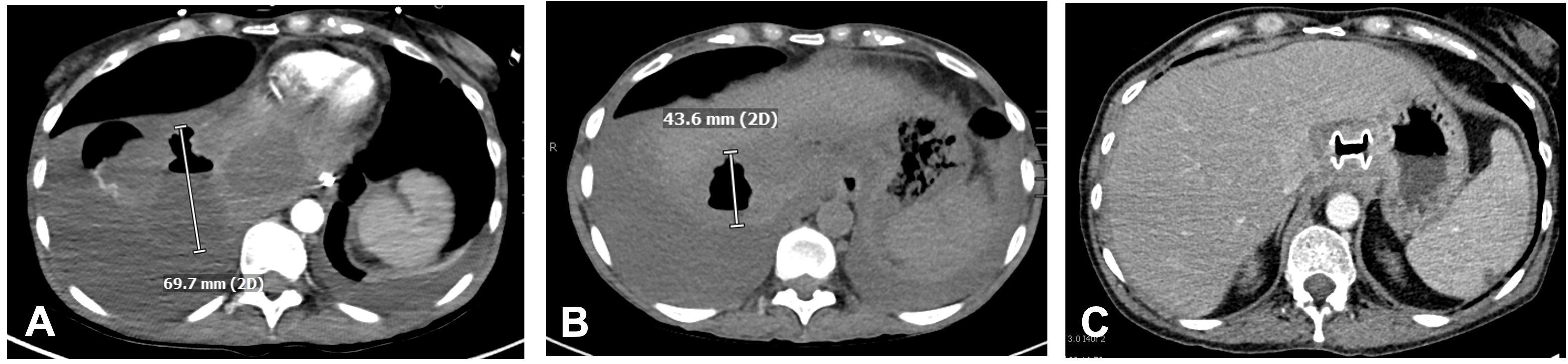
Case Description/Methods: A 50-year-old female with a history of alcohol related chronic pancreatitis presented to our hospital in severe respiratory distress requiring intubation for acute hypoxemic respiratory failure. A CT scan demonstrated a pseudocyst extending through the esophageal hiatus into the mediastinum and right lower lung where it measured 69.7mm. Multidisciplinary consensus between gastroenterology and interventional radiology was to proceed with EUS assisted creation of a cyst gastrostomy with placement of a metal stent.
A curvilinear echoendoscope was passed and advanced into the proximal stomach. Here, a 55mm anechoic cystic cavity with layering debris was brought into stable view. Using standard endo cut settings, a 10mm x 10mm lumen apposing axios metal stent was successfully placed using a cauterized technique. The echoendoscope was then exchanged for the gastroscope and the stent was seen to be in good position draining cystic fluid.
Four days after the procedure, a CT scan showed the stent extending from the proximal stomach to the pseudocyst, which had decreased in size from 69.7mm to 43.6mm. One week following the initial procedure, the patient underwent upper endoscopy, which showed the lumen-apposing metal stent in the cardia along with an empty cavity and scant fluid drainage when suction was applied through the stent. A CT scan performed 8 weeks later showed complete resolution of the pseudocyst. The patient then underwent upper endoscopy with EUS, which confirmed resolution of the pseudocyst and the stent was removed using rat tooth forceps.
Discussion: In this case, we have demonstrated the utility of EUS in the creation of a cyst gastrostomy to successfully treat a patient with acute respiratory failure secondary to pancreatic pseudocyst extension into the mediastinum and right lower lung. Further studies are needed to evaluate for pseudocyst recurrence following this procedure to determine its long-term efficacy in the management of mediastinal pseudocysts.
Disclosures:
Alexandra Kimchy, DO, William D. Davis, DO, Ahmad Nakshabandi, MD, Stanley Pietrak, MD, Walid Chalhoub, MD. C0198 - EUS-Guided Cyst Gastrostomy for Treatment of a Pancreatic Pseudocyst Extending Into the Mediastinum Resulting in Acute Respiratory Failure, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
MedStar Georgetown University Hospital, Washington, DC
Introduction: Mediastinal pseudocysts are the result of a rare drainage tract formation that develops more often in patients with a history of alcohol related chronic pancreatitis. The current evidence suggests favorable outcomes using endoscopic transmural drainage in the management of pancreatic pseudocysts. Here, we present a challenging approach to an unusual complication of a pancreatic pseudocyst extending into the mediastinum using EUS guided creation of a cyst gastrostomy.
Case Description/Methods: A 50-year-old female with a history of alcohol related chronic pancreatitis presented to our hospital in severe respiratory distress requiring intubation for acute hypoxemic respiratory failure. A CT scan demonstrated a pseudocyst extending through the esophageal hiatus into the mediastinum and right lower lung where it measured 69.7mm. Multidisciplinary consensus between gastroenterology and interventional radiology was to proceed with EUS assisted creation of a cyst gastrostomy with placement of a metal stent.
A curvilinear echoendoscope was passed and advanced into the proximal stomach. Here, a 55mm anechoic cystic cavity with layering debris was brought into stable view. Using standard endo cut settings, a 10mm x 10mm lumen apposing axios metal stent was successfully placed using a cauterized technique. The echoendoscope was then exchanged for the gastroscope and the stent was seen to be in good position draining cystic fluid.
Four days after the procedure, a CT scan showed the stent extending from the proximal stomach to the pseudocyst, which had decreased in size from 69.7mm to 43.6mm. One week following the initial procedure, the patient underwent upper endoscopy, which showed the lumen-apposing metal stent in the cardia along with an empty cavity and scant fluid drainage when suction was applied through the stent. A CT scan performed 8 weeks later showed complete resolution of the pseudocyst. The patient then underwent upper endoscopy with EUS, which confirmed resolution of the pseudocyst and the stent was removed using rat tooth forceps.
Discussion: In this case, we have demonstrated the utility of EUS in the creation of a cyst gastrostomy to successfully treat a patient with acute respiratory failure secondary to pancreatic pseudocyst extension into the mediastinum and right lower lung. Further studies are needed to evaluate for pseudocyst recurrence following this procedure to determine its long-term efficacy in the management of mediastinal pseudocysts.
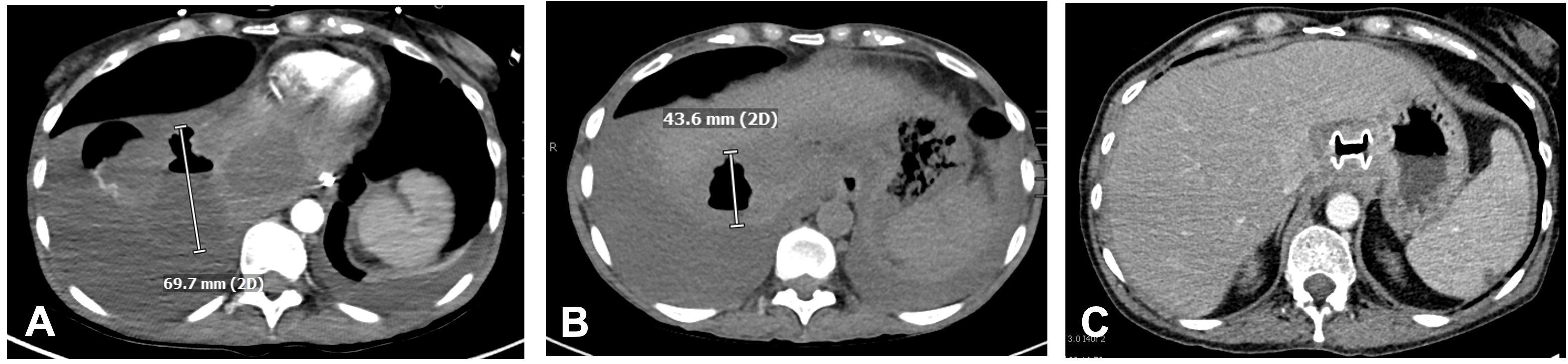
Figure: Figure 1: (A) CT scan showing a pseudocyst extending through the esophageal hiatus into the right lower lobe of the lung where it measured 69.7 mm and appeared to contain gas. (B) CT scan showing a stent extending from the stomach to the pseudocyst which decreased in size to 43.6 mm and an enlarging moderate right pleural effusion. (C) CT scan demonstrating the stent placed on prior admission with interval resolution of the previously demonstrated large pseudocyst.
Disclosures:
Alexandra Kimchy indicated no relevant financial relationships.
William Davis indicated no relevant financial relationships.
Ahmad Nakshabandi indicated no relevant financial relationships.
Stanley Pietrak indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Alexandra Kimchy, DO, William D. Davis, DO, Ahmad Nakshabandi, MD, Stanley Pietrak, MD, Walid Chalhoub, MD. C0198 - EUS-Guided Cyst Gastrostomy for Treatment of a Pancreatic Pseudocyst Extending Into the Mediastinum Resulting in Acute Respiratory Failure, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
