Back

Poster Session C - Monday Afternoon
Category: Esophagus
C0223 - The Evolution of TIF in 3 Eras
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Lana Aleuy, BS
Philadelphia College of Osteopathic Medicine
Suwanee, GA
Presenting Author(s)
Lana Aleuy, BS1, Aliu Sanni, MD2, Glenn Ihde, MD3
1Philadelphia College of Osteopathic Medicine, Suwanee, GA; 2Eastside Bariatric and General Surgery LLC, Snellville, GA; 3Matagorda Medical Group, Bay City, TX
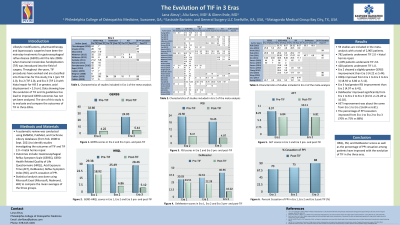
Introduction: Lifestyle modifications, pharmacotherapy, and laparoscopic surgeries have been the mainstay treatments for gastroesophageal reflux disease (GERD) until the late 2000s when transoral incisionless fundoplication (TIF) was introduced into the field of surgery. Throughout the years, TIF procedures have evolved and are classified into three Eras for this study; Era 1 (pre TIF 2.0), Era 2 (TIF 2.0), and Era 3 (TIF 2.0 with hiatal repair for Hill 3 or greater, axial displacement > 2.0 cm). Data showing how the evolution of TIF and its guidelines has led to improved GERD outcomes has not yet been analyzed. The aim of this study is to evaluate and compare the outcomes of TIF in three ERAs.
Methods: A systematic review was conducted using EMBASE, PubMed, and Cochrane Library databases (from Feb. 2008 to Sept. 2021) to identify studies investigating the outcomes of TIF and TIF with concomitant hiatal hernia repair. The outcomes analyzed include gastroesophageal reflux symptom scale (GERSS), GERD health related quality of life questionnaire (GERD-HRQL), acid exposure time (AET), DeMeester, reflux symptom index (RSI), and percentage of PPI cessation. Results are expressed as differences in means with standard deviation (SD) and odds ratio (OR). Statistical analysis was done using Microsoft Excel (Microsoft, Redmond, WA) to compare the mean averages of the three groups.
Results: Fifty-nine studies were quantitatively assessed and included in this meta-analysis. A total of 2,905 patients were included; 782 patients who underwent TIF 2.0 with concomitant hiatal hernia repair, 1,695 patients who underwent TIF 2.0, and 428 patients who underwent TIF 1.0.
Era 2 had a slightly greater GERSS improvement than Era 3 (4.22 vs 5.44).
HRQL improved from Era 1 to Era 2 to Era 3 (18.92 vs 6.86 vs 5.12).
Era 3 showed greater RSI improvement than Era 2 (4.97 vs 6.41).
DeMeester improved significantly from Era 1 to Era 2 to Era 3 (24.51 vs 22.28 vs 10.02).
AET improvement was about the same from Era 1 to Era 2 (6.84 vs 6.81).
The percentage of PPI cessation improved from Era 1 to Era 2 to Era 3 (70% vs 75% vs 88%).
Discussion: HRQL, RSI, and DeMeester scores as well as the percentage of PPI cessation among patients have improved with the evolution of TIF in the three Eras.

Disclosures:
Lana Aleuy, BS1, Aliu Sanni, MD2, Glenn Ihde, MD3. C0223 - The Evolution of TIF in 3 Eras, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Philadelphia College of Osteopathic Medicine, Suwanee, GA; 2Eastside Bariatric and General Surgery LLC, Snellville, GA; 3Matagorda Medical Group, Bay City, TX
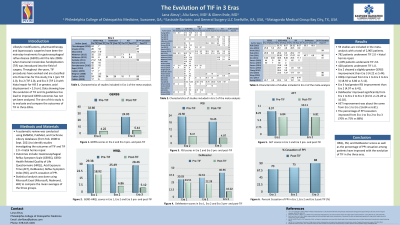
Introduction: Lifestyle modifications, pharmacotherapy, and laparoscopic surgeries have been the mainstay treatments for gastroesophageal reflux disease (GERD) until the late 2000s when transoral incisionless fundoplication (TIF) was introduced into the field of surgery. Throughout the years, TIF procedures have evolved and are classified into three Eras for this study; Era 1 (pre TIF 2.0), Era 2 (TIF 2.0), and Era 3 (TIF 2.0 with hiatal repair for Hill 3 or greater, axial displacement > 2.0 cm). Data showing how the evolution of TIF and its guidelines has led to improved GERD outcomes has not yet been analyzed. The aim of this study is to evaluate and compare the outcomes of TIF in three ERAs.
Methods: A systematic review was conducted using EMBASE, PubMed, and Cochrane Library databases (from Feb. 2008 to Sept. 2021) to identify studies investigating the outcomes of TIF and TIF with concomitant hiatal hernia repair. The outcomes analyzed include gastroesophageal reflux symptom scale (GERSS), GERD health related quality of life questionnaire (GERD-HRQL), acid exposure time (AET), DeMeester, reflux symptom index (RSI), and percentage of PPI cessation. Results are expressed as differences in means with standard deviation (SD) and odds ratio (OR). Statistical analysis was done using Microsoft Excel (Microsoft, Redmond, WA) to compare the mean averages of the three groups.
Results: Fifty-nine studies were quantitatively assessed and included in this meta-analysis. A total of 2,905 patients were included; 782 patients who underwent TIF 2.0 with concomitant hiatal hernia repair, 1,695 patients who underwent TIF 2.0, and 428 patients who underwent TIF 1.0.
Era 2 had a slightly greater GERSS improvement than Era 3 (4.22 vs 5.44).
HRQL improved from Era 1 to Era 2 to Era 3 (18.92 vs 6.86 vs 5.12).
Era 3 showed greater RSI improvement than Era 2 (4.97 vs 6.41).
DeMeester improved significantly from Era 1 to Era 2 to Era 3 (24.51 vs 22.28 vs 10.02).
AET improvement was about the same from Era 1 to Era 2 (6.84 vs 6.81).
The percentage of PPI cessation improved from Era 1 to Era 2 to Era 3 (70% vs 75% vs 88%).
Discussion: HRQL, RSI, and DeMeester scores as well as the percentage of PPI cessation among patients have improved with the evolution of TIF in the three Eras.
Disclosures:
Lana Aleuy indicated no relevant financial relationships.
Aliu Sanni indicated no relevant financial relationships.
Glenn Ihde indicated no relevant financial relationships.
Lana Aleuy, BS1, Aliu Sanni, MD2, Glenn Ihde, MD3. C0223 - The Evolution of TIF in 3 Eras, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
