Back
Poster Session D - Tuesday Morning
D0604 - A Case of Drug-Induced Liver Injury Secondary to Clobenzorex Use
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
.jpg)
Ushan A. Ranasinghe, MS, MD
Swedish Hospital
Chicago, IL
Presenting Author(s)
Ushan A. Ranasinghe, MS, MD1, Syed I. Hussaini, DO1, Michael Gianarakis, BSc2, Eduardo Villa, MD1
1Swedish Hospital, Chicago, IL; 2St. George's University of London, Chicago, IL
Introduction: Drug-induced liver injury (DILI) is a cause of both acute and chronic liver disease and is often a challenging condition for clinicians. It is a diagnosis of exclusion that requires a detailed history and workup to ensure other potential causes have been ruled out before affirming the diagnosis. There are numerous offending agents with varied presentations, often idiosyncratic in nature, with the additional challenge being a lack of specific testing or biomarkers to aid diagnosis.
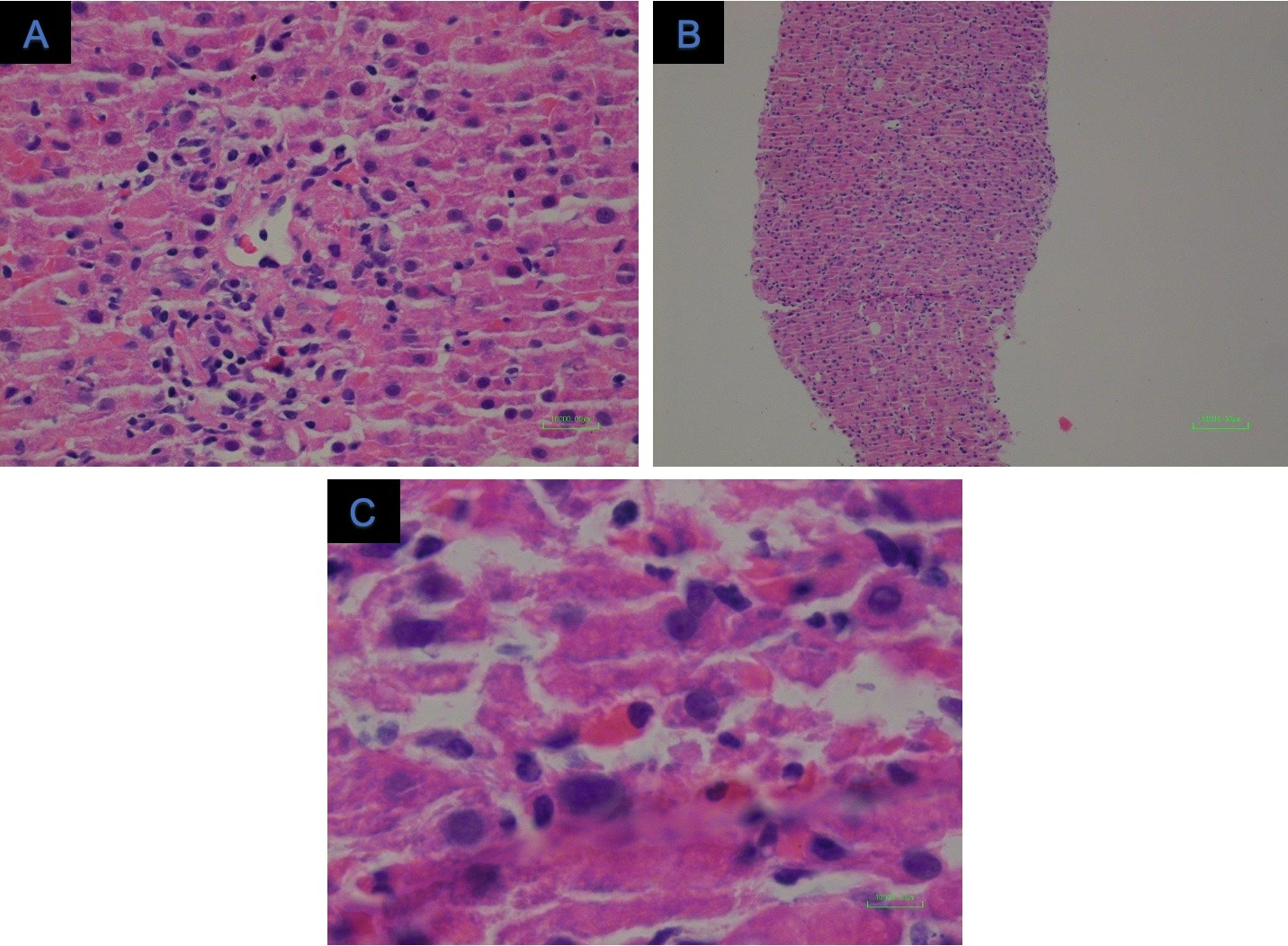
Case Description/Methods: We present a case of a 25-year-old male who immigrated from Mexico 4 months ago, with no reported past medical history, who presented to the emergency department for a two-day history of postprandial non-radiating right upper quadrant and epigastric pain. Associated symptoms include subjective fevers, chills, decreased appetite, nausea, one episode of blood-tinged emesis, night sweats and dyspnea. The patient worked as a driver in Mexico and was taking two different formulations of 30mg Clobenzorex, an amphetamine pro-drug, daily for two years to help him stay awake for work. These medications were available over the counter. He had not taken it since he moved to the US. He denies the use of illicit drugs, contact with any inmates or Tuberculosis patients. At the time of his presentation, he works in a wooden floor-making company. Labs revealed a markedly elevated total bilirubin of 4.4 mg/dL, INR 1.1, AST 1325 IU/L, ALT 3151 IU/L, LDH 745 IU/L and a mildly elevated ALP 220 IU/L. Acute hepatitis and autoimmune panels were not reactive. Serum acetaminophen level was also within normal limits. Ultrasound of the abdomen and MRCP noted gallbladder wall thickening but no biliary dilatation or pathology. The patient subsequently underwent a core-needle liver biopsy that displayed lobular infiltrates of inflammatory cells of predominantly lymphocytes (Figure 1). Given the absence of positive viral serology, a diagnosis of drug-induced hepatitis was concluded.
Discussion: This case report documents a unique instance of drug-induced liver injury secondary to Clobenzorex use. This case highlights the importance of a detailed social history and should encourage clinicians not to neglect to ask about over-the-counter medications to help elucidate potential causes of liver injury. This is an important consideration, especially in the subset of patients from countries outside the United States who have access to a variety of OTC medications that are potentially hepatotoxic.
Disclosures:
Ushan A. Ranasinghe, MS, MD1, Syed I. Hussaini, DO1, Michael Gianarakis, BSc2, Eduardo Villa, MD1. D0604 - A Case of Drug-Induced Liver Injury Secondary to Clobenzorex Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Swedish Hospital, Chicago, IL; 2St. George's University of London, Chicago, IL
Introduction: Drug-induced liver injury (DILI) is a cause of both acute and chronic liver disease and is often a challenging condition for clinicians. It is a diagnosis of exclusion that requires a detailed history and workup to ensure other potential causes have been ruled out before affirming the diagnosis. There are numerous offending agents with varied presentations, often idiosyncratic in nature, with the additional challenge being a lack of specific testing or biomarkers to aid diagnosis.
Case Description/Methods: We present a case of a 25-year-old male who immigrated from Mexico 4 months ago, with no reported past medical history, who presented to the emergency department for a two-day history of postprandial non-radiating right upper quadrant and epigastric pain. Associated symptoms include subjective fevers, chills, decreased appetite, nausea, one episode of blood-tinged emesis, night sweats and dyspnea. The patient worked as a driver in Mexico and was taking two different formulations of 30mg Clobenzorex, an amphetamine pro-drug, daily for two years to help him stay awake for work. These medications were available over the counter. He had not taken it since he moved to the US. He denies the use of illicit drugs, contact with any inmates or Tuberculosis patients. At the time of his presentation, he works in a wooden floor-making company. Labs revealed a markedly elevated total bilirubin of 4.4 mg/dL, INR 1.1, AST 1325 IU/L, ALT 3151 IU/L, LDH 745 IU/L and a mildly elevated ALP 220 IU/L. Acute hepatitis and autoimmune panels were not reactive. Serum acetaminophen level was also within normal limits. Ultrasound of the abdomen and MRCP noted gallbladder wall thickening but no biliary dilatation or pathology. The patient subsequently underwent a core-needle liver biopsy that displayed lobular infiltrates of inflammatory cells of predominantly lymphocytes (Figure 1). Given the absence of positive viral serology, a diagnosis of drug-induced hepatitis was concluded.
Discussion: This case report documents a unique instance of drug-induced liver injury secondary to Clobenzorex use. This case highlights the importance of a detailed social history and should encourage clinicians not to neglect to ask about over-the-counter medications to help elucidate potential causes of liver injury. This is an important consideration, especially in the subset of patients from countries outside the United States who have access to a variety of OTC medications that are potentially hepatotoxic.
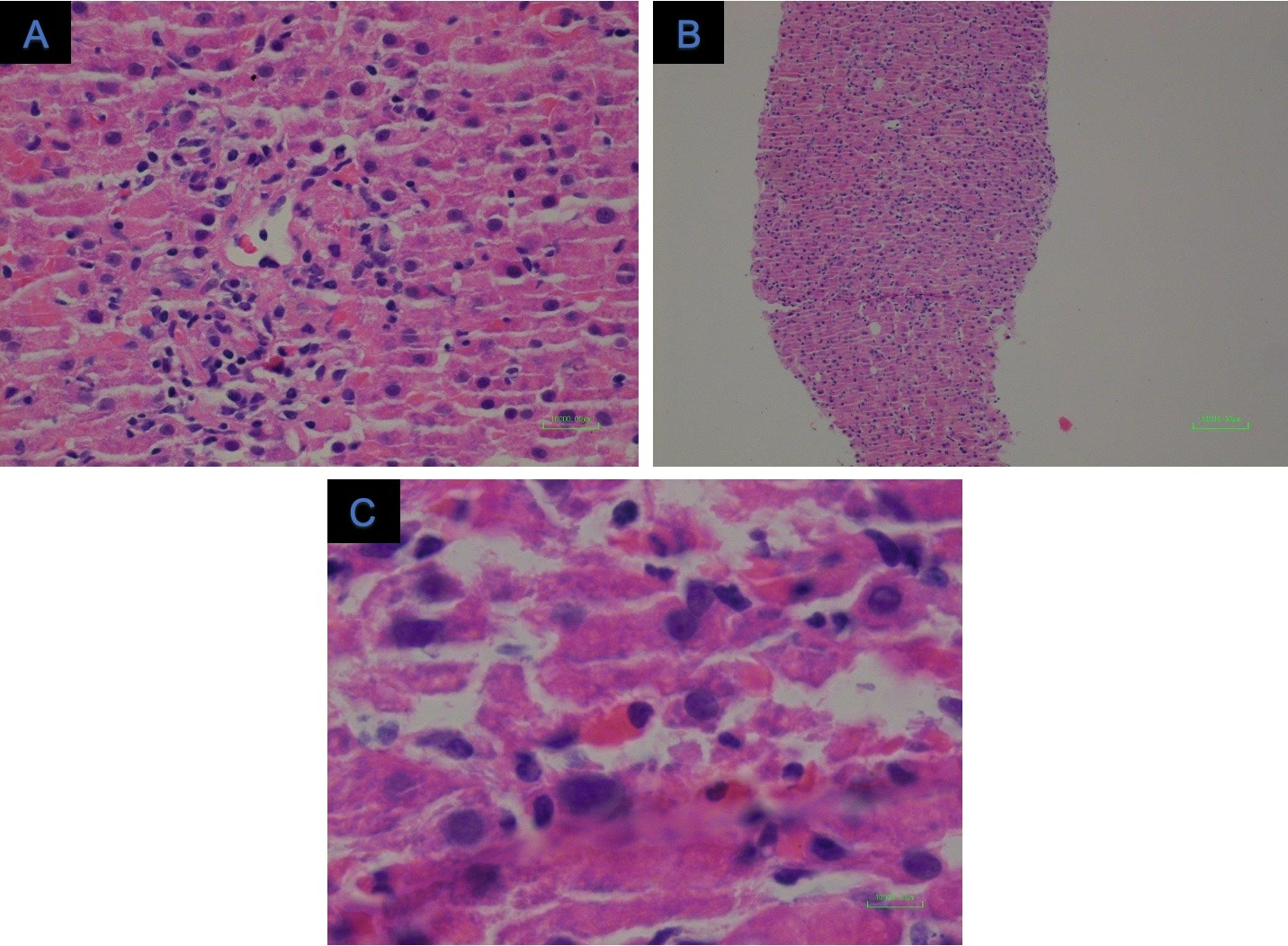
Figure: Figure 1: Core needle liver biopsy showing lobular infiltrates of inflammatory cells consisting of predominantly lymphocytes.
Disclosures:
Ushan Ranasinghe indicated no relevant financial relationships.
Syed Hussaini indicated no relevant financial relationships.
Michael Gianarakis indicated no relevant financial relationships.
Eduardo Villa indicated no relevant financial relationships.
Ushan A. Ranasinghe, MS, MD1, Syed I. Hussaini, DO1, Michael Gianarakis, BSc2, Eduardo Villa, MD1. D0604 - A Case of Drug-Induced Liver Injury Secondary to Clobenzorex Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
