Back
Poster Session B - Monday Morning
B0293 - Ischemic Gastritis With Gastric Pneumatosis and Portal Venous Gas
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Kwabena O. Adu-Gyamfi, MBChB
Medical College of Georgia - Augusta University
Augusta, GA
Presenting Author(s)
Kwabena O. Adu-Gyamfi, MBChB1, Dominic Amakye, MBChB2, Praneeth Kudaravalli, MD3, Dariush Shahsavari, MD1, John Erikson L. Yap, MD4
1Medical College of Georgia - Augusta University, Augusta, GA; 2Piedmont Athens Regional Medical Center, Athens, GA; 3Augusta University Medical Center, Augusta, GA; 4Augusta University Medical College of Georiga, Augusta, GA
Introduction: Gastric ischemia is rare due to extensive collateral blood supply to the stomach, but if it occurs is associated with poor prognosis. We present the case of acute severe gastric ischemia in the context of severe hypotension with demonstration of portal venous gas (PVG) and gastric wall pneumatosis. The inciting event was a suspected gastric volvulus which had spontaneously resolved by the time of radiologic and endoscopic evaluation. This case highlights the successful conservative management of this dreaded clinical condition.
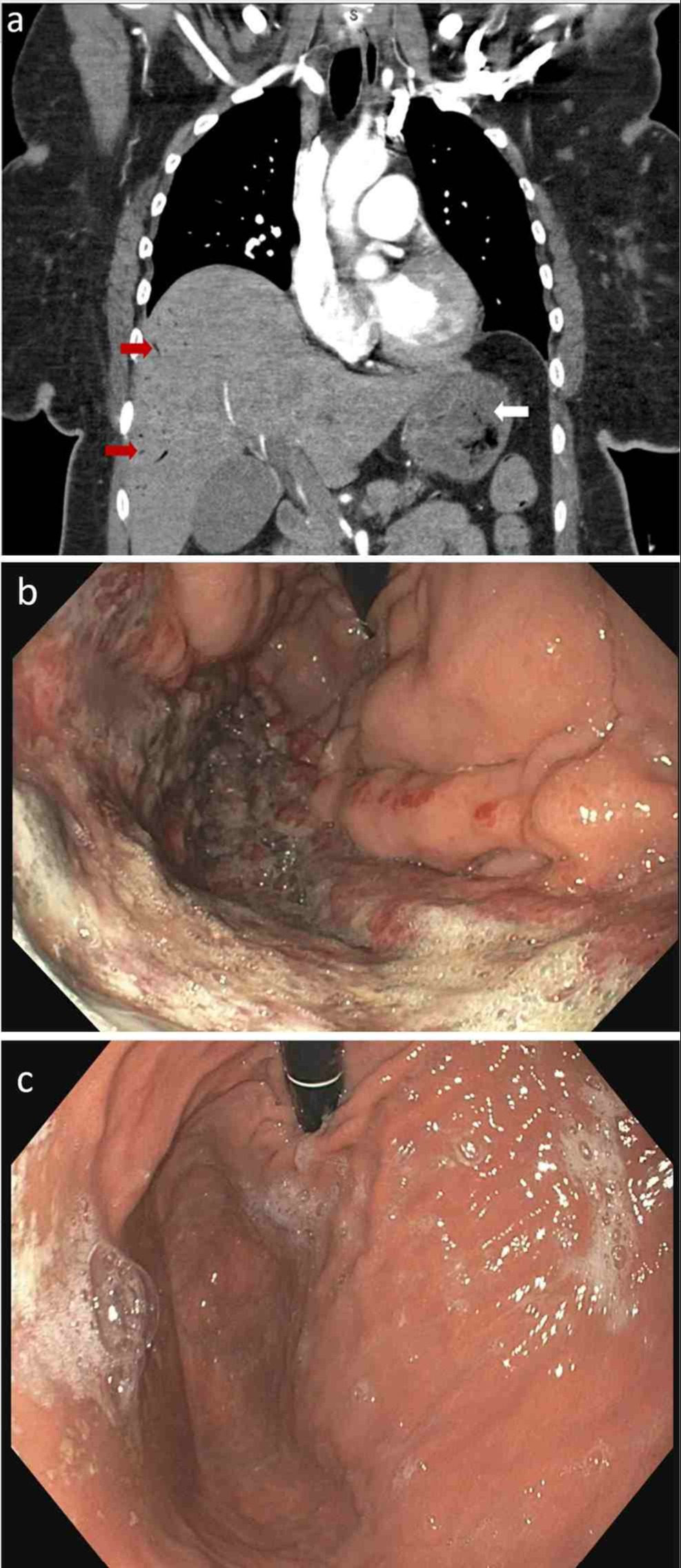
Case Description/Methods: A 50-year-old African American woman presented to the emergency department with 1-day history of severe lower retrosternal and epigastric pain with persistent nausea, coffee ground emesis and retching. Examination revealed an ill-appearing, tachycardic, hypotensive (blood pressure 70/41mmHg) female with epigastric tenderness. The rest of vitals, physical exam, EKG and chest x-ray were normal. Basic labs after initial fluid resuscitation noted WBC of 12.5x109/L. Troponin, electrolytes, liver enzymes and lactic acid were normal. Chest CT angiogram showed peripheral hepatic PVG (Fig 1a, red arrows) and a thickened gastric wall with pneumatosis (Fig 1a, white arrow) suggestive of gastric ischemia. No evidence of pulmonary embolism, bowel perforation or vascular abnormality was found. Esophagogastroduodenoscopy (EGD) revealed extensive necrotic ulcerative changes along gastric greater curvature from fundus to body consistent with gastric ischemia (Fig 1b). Treatment included intravenous fluids and proton pump inhibitors, analgesics, IV antibiotics (ceftriaxone and metronidazole) and bowel rest. Patient responded well to treatment and was discharged home after six days. Patient remained asymptomatic and a repeat EGD after 12 weeks revealed completely normal appearance of stomach (Fig 1c).
Discussion: Gastric ischemia may be caused by local vascular abnormalities, systemic hypoperfusion and mechanical obstruction. Typical symptoms include abdominal pain, vomiting and gastric bleeding. The mechanism for developing PVG in bowel ischemia is not fully understood but usually suggests an ominous pathology which may require a prompt surgical intervention. Transient gastric volvulus was suspected as a possible initial trigger, causing hypotension and gastric ischemia as no other etiology was identified. Enhanced provider cognizance of gastric ischemia and appropriate management tailored to each patient’s needs should improve clinical outcomes.
Disclosures:
Kwabena O. Adu-Gyamfi, MBChB1, Dominic Amakye, MBChB2, Praneeth Kudaravalli, MD3, Dariush Shahsavari, MD1, John Erikson L. Yap, MD4. B0293 - Ischemic Gastritis With Gastric Pneumatosis and Portal Venous Gas, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Medical College of Georgia - Augusta University, Augusta, GA; 2Piedmont Athens Regional Medical Center, Athens, GA; 3Augusta University Medical Center, Augusta, GA; 4Augusta University Medical College of Georiga, Augusta, GA
Introduction: Gastric ischemia is rare due to extensive collateral blood supply to the stomach, but if it occurs is associated with poor prognosis. We present the case of acute severe gastric ischemia in the context of severe hypotension with demonstration of portal venous gas (PVG) and gastric wall pneumatosis. The inciting event was a suspected gastric volvulus which had spontaneously resolved by the time of radiologic and endoscopic evaluation. This case highlights the successful conservative management of this dreaded clinical condition.
Case Description/Methods: A 50-year-old African American woman presented to the emergency department with 1-day history of severe lower retrosternal and epigastric pain with persistent nausea, coffee ground emesis and retching. Examination revealed an ill-appearing, tachycardic, hypotensive (blood pressure 70/41mmHg) female with epigastric tenderness. The rest of vitals, physical exam, EKG and chest x-ray were normal. Basic labs after initial fluid resuscitation noted WBC of 12.5x109/L. Troponin, electrolytes, liver enzymes and lactic acid were normal. Chest CT angiogram showed peripheral hepatic PVG (Fig 1a, red arrows) and a thickened gastric wall with pneumatosis (Fig 1a, white arrow) suggestive of gastric ischemia. No evidence of pulmonary embolism, bowel perforation or vascular abnormality was found. Esophagogastroduodenoscopy (EGD) revealed extensive necrotic ulcerative changes along gastric greater curvature from fundus to body consistent with gastric ischemia (Fig 1b). Treatment included intravenous fluids and proton pump inhibitors, analgesics, IV antibiotics (ceftriaxone and metronidazole) and bowel rest. Patient responded well to treatment and was discharged home after six days. Patient remained asymptomatic and a repeat EGD after 12 weeks revealed completely normal appearance of stomach (Fig 1c).
Discussion: Gastric ischemia may be caused by local vascular abnormalities, systemic hypoperfusion and mechanical obstruction. Typical symptoms include abdominal pain, vomiting and gastric bleeding. The mechanism for developing PVG in bowel ischemia is not fully understood but usually suggests an ominous pathology which may require a prompt surgical intervention. Transient gastric volvulus was suspected as a possible initial trigger, causing hypotension and gastric ischemia as no other etiology was identified. Enhanced provider cognizance of gastric ischemia and appropriate management tailored to each patient’s needs should improve clinical outcomes.
Figure: Fig. 1. Chest CT angiogram showed peripheral hepatic PVG (Fig 1a, red arrows) and a thickened gastric wall with pneumatosis (Fig 1a, white arrow). EGD showing extensive necrotic ulcerative changes along gastric greater curvature from fundus to body (Fig 1b). EGD after 12 weeks showing normal stomach (Fig 1c)
Disclosures:
Kwabena Adu-Gyamfi indicated no relevant financial relationships.
Dominic Amakye indicated no relevant financial relationships.
Praneeth Kudaravalli indicated no relevant financial relationships.
Dariush Shahsavari indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Kwabena O. Adu-Gyamfi, MBChB1, Dominic Amakye, MBChB2, Praneeth Kudaravalli, MD3, Dariush Shahsavari, MD1, John Erikson L. Yap, MD4. B0293 - Ischemic Gastritis With Gastric Pneumatosis and Portal Venous Gas, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
